'People will forgive you for being wrong, but they will never forgive you for being right - especially if events prove you right while proving them wrong.' Thomas Sowell
Search This Blog
Saturday, 19 August 2023
Thursday, 27 July 2023
Monday, 5 December 2022
Does religious faith lead to a happier, healthier life?
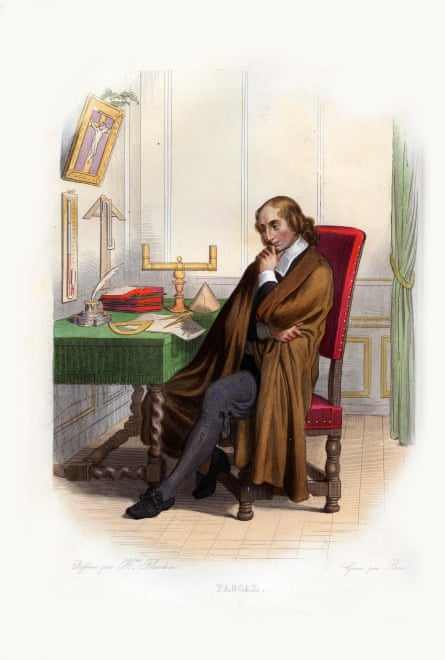
In his Pensées, published posthumously in 1670, the French philosopher Blaise Pascal appeared to establish a foolproof argument for religious commitment, which he saw as a kind of bet. If the existence of God was even minutely possible, he claimed, then the potential gain was so huge – an “eternity of life and happiness” – that taking the leap of faith was the mathematically rational choice.
Pascal’s wager implicitly assumes that religion has no benefits in the real world, but some sacrifices. But what if there were evidence that faith could also contribute to better wellbeing? Scientific studies suggest this is the case. Joining a church, synagogue or temple even appears to extend your lifespan.
These findings might appear to be proof of divine intervention, but few of the scientists examining these effects are making claims for miracles. Instead, they are interested in understanding the ways that it improves people’s capacity to deal with life’s stresses. “Religious and spiritual traditions give you access to different methods of coping that have distinctive benefits,” says Doug Oman, a professor in public health at the University of California Berkeley. “From the psychological perspective, religions offer a package of different ingredients,” agrees Prof Patty Van Cappellen at Duke University in Durham, North Carolina.
Studying the life-extending benefits of religious practice can therefore offer useful strategies for anyone – of any faith or none – to live a healthier and happier life. You may find yourself shaking your head in scepticism, but the evidence base linking faith to better health has been decades in the making and now encompasses thousands of studies. Much of this research took the form of longitudinal research, which involves tracking the health of a population over years and even decades. They each found that measures of someone’s religious commitment, such as how often they attended church, were consistently associated with a range of outcomes, including a lower risk of depression, anxiety and suicide and reduced cardiovascular disease and death from cancer.

Unlike some other areas of scientific research suffering from the infamous “replication crisis”, these studies have examined populations across the globe, with remarkably consistent results. And the effect sizes are large. Dr Laura Wallace at the University of Chicago Booth School of Business, for instance, recently examined obituaries of more than 1,000 people across the US and looked at whether the article recorded the person’s religious affiliation – a sign that their faith had been a major element of their identity.
Publishing her results in 2018, she reported that those people marked out for their faith lived for 5.6 years more, on average, than those whose religion had not been recorded; in a second sample, looking specifically at a set of obituaries from Des Moines in Iowa, the difference was even greater – about 10 years in total. “It’s on par with the avoidance of major health risks – like smoking,” says Wallace. To give another comparison: reducing hypertension adds about five years to someone’s life expectancy.
Health effects of this size demand explanation and scientists such as Wallace have been on the case. One obvious explanation for these findings is that people of faith live cleaner lives than the non-religious: studies show that churchgoers are indeed less likely to smoke, drink, take drugs or practise unsafe sex than people who do not attend a service regularly (though there are, of course, notable exceptions).
This healthier living may be the result of the religious teaching itself, which tends to encourage the principles of moderation and abstinence. But it could also be the fact that religious congregations are a self-selecting group. If you have sufficient willpower to get out of bed on a Sunday morning, for example, you may also have enough self-control to resist life’s other temptations.
Importantly, however, the health benefits of religion remain even when the scientists have controlled for these differences in behaviour, meaning that other factors must also contribute. Social connection comes top of the list. Feelings of isolation and loneliness are a serious source of stress in themselves and exacerbate the other challenges we face in life. Even something as simple as getting to work becomes far more difficult if you cannot call on a friend to give you a lift when your car breaks down.
Chronic stress response can result in physiological changes such as heightened inflammation, which, over the years, can damage tissue and increase your risk of illness. As a result, the size of someone’s social network and their subjective sense of connection with others can both predict their health and longevity, with one influential study by Prof Julianna Holt-Lunstad at Brigham Young University suggesting that the influence of loneliness is comparable to that of obesity or low physical exercise.
Religions, of course, tend to be built around a community of like-minded worshippers who meet regularly and have a shared set of beliefs. And many of the specific rituals will also contribute to a sense of communion with others. Christians, for example, are encouraged to pray on behalf of other people and this seems to bring its own health benefits, according to a brand new study by Prof Gail Ironson at the University of Miami.
Ironson has spent decades studying the ways that people with HIV cope with their infection and the influences of these psychological factors on the outcomes of disease. Examining data covering 17 years of 102 HIV patients’ lives, she found that people who regularly prayed for others were twice as likely to survive to the end of the study, compared with those who more regularly prayed for themselves. Importantly, the link remained even after Ironson had accounted for factors such as adherence to medications or substance abuse or the patient’s initial viral load.
Besides encouraging social connection, religion can help people to cultivate positive emotions that are good for our mental and physical wellbeing, such as gratitude and awe. Various studies show that regularly counting your blessings can help you to shift your focus away from the problems you are facing, preventing you from descending into the negative spirals of thinking that amplify stress. In the Christian church, you may be encouraged to thank God in your prayers, which encourages the cultivation of this protective emotion. “It’s a form of cognitive reappraisal,” says Van Cappellen. “It’s helping you to re-evaluate your situation in a more positive light.”
Awe, meanwhile, is the wonder we feel when we contemplate something much bigger and more important than ourselves. This can help people to cut through self-critical, ruminative thinking and to look beyond their daily concerns, so that they no longer make such a dent on your wellbeing.
Last, but not least, religious faiths can create a sense of purpose in someone’s life – the feeling that there is a reason and meaning to their existence. People with a sense of purpose tend to have better mental wellbeing, compared with those who feel that their lives lack direction, and – once again – this seems to have knock-on effects for physical health, including reduced mortality. “When people have a core set of values, it helps establish goals. And when those goals are established and pursued, that produces better psychological wellbeing,” says Prof Eric Kim at the University of British Columbia, who has researched the health benefits of purpose in life. Much like awe and gratitude, those positive feelings can then act as a buffer to stress.

These are average effects, which don’t always take into account that huge variety of people’s experiences. While some Christians might see God as a benevolent figure, others might have been taught that he is judgmental and punishing and those views can make a big difference in the effects on our health. In her studies of HIV patients, Ironson found that people who believed in a vengeful God showed a faster disease progression – as measured by their declining white blood cell count – compared with those who believed that he was a merciful figure.
Ultimately, most people’s faith will arise from real convictions; it seems unlikely that many people would adopt a particular religious view solely for the health benefits. But even if you are agnostic, like me, or atheist, this research might inform your lifestyle.
You can start by considering contemplative techniques, which come in many more forms than the mindful breathing and body-scan techniques that have proved so popular. Scientists have become increasingly interested in “loving-kindness meditation”, for example, in which you spend a few moments thinking warm thoughts about friends, strangers, even enemies. The practice was inspired by the Buddhist principle of mettā, but it also resembles the Christian practice of intercessory prayer. When practised regularly, this increases people’s feelings of social connection and empathy with the consequent benefits for their mental health. Importantly, it also changes people’s real-life actions towards others, for instance encouraging more pro-social behaviour.
The power of religion is that it gives you this package of ingredients that are pre-made and organised for youProf Patty Van Cappellen
To build more gratitude into your life, meanwhile, you might keep a diary listing the things that you have appreciated each day and you can make a deliberate habit of thanking the people who have helped you; both strategies have been shown to improve people’s stress responses and to improve overall wellbeing. And to cultivate awe, you might go on a regular nature walk, visit a magnificent building within your city or watch a film that fills you with wonder.
If you have time and resources for greater commitments, you could also take up a voluntary activity for a cause that means a lot to you, a task that may help to boost your sense of purpose and which could also enhance your social life. Dr Wallace’s work has shown that the sheer amount of volunteering someone performs could, independently, explain part of the longevity boost of religious people, but charitable actions do not need to be linked to a particular faith for you to gain those benefits. “If people are able to plug into causes that really light up their intrinsic values, and then find a community that helps them reach their goals, that’s another way in which the framework of religion can be taken into a non-religious context,” says Prof Kim.
The challenge is to ensure that you build all these behaviours into your routine, so that you perform them with the same regularity and devotion normally reserved for spiritual practices. “The power of religion is that it gives you this package of ingredients that are pre-made and organised for you,” says Van Cappellen. “And if you are not religious you have to create it on your own.” You don’t need to make a leap of faith to see those benefits.
Wednesday, 26 October 2022
Friday, 12 August 2022
Sunday, 8 May 2022
Wednesday, 9 February 2022
Sunday, 9 January 2022
Wednesday, 28 July 2021
Monday, 12 July 2021
Monday, 24 May 2021
Sunday, 23 May 2021
Thursday, 6 May 2021
Sunday, 2 May 2021
Thursday, 24 December 2020
Covid prompts a new approach to economic growth
An FT Editorial
The coronavirus pandemic means that 2020 will go down in history as the year with one of the deepest plunges in national income on record. In the UK, which has one of the longest continuous logs of economic output, gross domestic product looks likely to have fallen around a tenth this year, making for the biggest recession in three centuries. Yet even these figures, however eye-watering, do not capture the true collapse in wellbeing, which must be the ultimate goal of economic policy.
In theory, gross domestic product adds up everything that a country produces in one year. The fall in national income during 2020 is easy to explain: interruptions to normal economic activity have meant that far less has been produced. In this regard the drop in gross domestic product will capture some of the missed outings and trips to the cinema, the cancelled holidays and all the meals and drinks with friends that had to be postponed.
There is, however, plenty that the figures miss. To aggregate the value of very different activities that take place in an economy statisticians use market prices — allowing them to compare the production of both apples and oranges on a common scale. But the absence of these prices for much of healthcare and education in many countries — statisticians merely impute their production from how much the government spends on them — means the disruptions to schools and delays in administering non-coronavirus medical care is missed. Spending on healthcare might have risen but on a net basis societies got far less for their money.
On the other hand, public parks and other green spaces have become much more important but their contribution to the economy will not be registered as part of GDP. Unpaid labour too, those who tried to teach their children at home, sewed personal protective equipment or baked banana bread, will not appear in the story of the year told by national income figures. Nor will the drop in air pollution or the volunteers who took care of neighbours.
Even an accurate counting of the drop in production this year would still miss the psychological damage done by prolonged isolation and loneliness; the “hidden pandemic” of mental health problems. That suggests the solution would not be to expand the definition of gross domestic product to include the production it misses but to consider focusing on wellbeing directly.
All the same, the experience of this year — when governments shut down their economies in order to protect public health — has shown that economic growth has not been prioritised above all else. Already, a wider definition of wellbeing than a pure economic one is implicitly being used to inform policy. Daily count cases and death rates have played a much bigger role in policymaking than quarterly growth figures. Suggestions that health measures represent a trade-off with economic fortunes have also been overplayed. The best way of protecting jobs this year has been keeping the virus under control: New Zealand, which managed to remain virtually virus-free thanks to an early and strict lockdown, is reaping the economic rewards.
This will remain true when the pandemic has passed. A healthy and well-educated workforce is one of the most important prerequisites to growth and secure, well-paid, high quality jobs are among the best foundations to protect mental wellbeing. Unemployment and poor-quality work can easily destroy people’s sense of self-worth while a robust private sector is essential to provide the tax revenues for health and education. The goal should be to create the kind of society where economic growth and wellbeing go hand in hand.
Wednesday, 20 May 2020
Returning to work in the coronavirus crisis: what are your rights?
As the lockdown restrictions begin to be eased across the UK, more workers are being asked to return to the workplace.
The government has said that employees should only be asked to go back if they cannot do their job from home, so if you can, your employer should not be asking you to travel in to work.
If you do need to go to your workplace, your employer is obliged to make sure you will be safe there. Employment lawyer Matt Gingell says: “Employers have a general duty to ensure, as far as reasonably practicable, the health, safety and welfare of all of their employees.”
Here’s a guide to your rights if your employer wants you back in the workplace.
How much notice should I be given that I have to return?
“If employees are unable to work from home, employers can ask employees to return to work and, technically, no notice is required,” says Gingell.
Solicitor and consumer law expert Gary Rycroft says there is no notice period written into law “but giving at least 48 hours’ notice should allow either side to have discussions and air any concerns or even official ‘grievances’”.
The advisory group Acas says employers need to check if there are any arrangements in place with unions or similar about notice. It advises: “Employees and workers should be ready to return to work at short notice, but employers should be flexible where possible.”
So while your employer could ask you to return straight away, a good employer would understand if there were things you needed to put in place first, and give you chance to do so.
What if I was furloughed?
When you were furloughed your employer should have outlined what would happen when it wanted you to go back to work, and this may have a clause saying that you have to return as soon as you are asked.
“The termination of the furlough agreement and when an employee will be expected to return to work will depend on the provisions of the agreement,” says Gingell. Again, though, even if there is no notice period, a good employer should realise that you may need some time to prepare.
If you have been furloughed under the government’s job retention scheme, your employer can’t ask you to go in and do ad hoc days, or work part-time. They would need to take you off furlough and renegotiate your contract with you.
Can they ask me to go back in part-time?
Not, currently, if you have been furloughed and they are using the government scheme to pay you. It only allows companies to furlough people for all of their normal hours, and bans them from asking you to do any work while you are off.
But if your company has not claimed government money to cover your wages, it can ask you to resume work part-time. Make sure you understand the terms of the request – your employer cannot adjust your contract without your permission, so if it is asking you to change your hours you should get advice.
Can they ask me to take a pay cut?
“The law here is the same as it would be if an employer made the same request in the normal course of an employee’s employment. Reducing hours and/or pay are deemed to be such fundamental changes to an employee’s terms and conditions that the employee concerned should be consulted and then agree in writing,” says Rycroft.
He points out that for some employers “this may be the only economically viable option”, and the alternative, if people refuse, could be redundancies. To make more than 20 people redundant there will need to be collective consultation.
What if I am in a vulnerable group or live with someone who is?
No special rules have been put in place to protect people in these groups who are asked to go into work but some already exist – if you are disabled or pregnant, for example, your employer has extra obligations.
Rycroft says some employees may be able to argue that it will be discriminatory to force them to attend work outside the home. “It is all a question of degrees, in terms of how the employer can show that they have listened to legitimate concerns and made reasonable adjustments,” he says.
If you are pregnant your employer is obliged to make sure you can do your job safely. This can mean allowing you to do your job from home, or giving you a new role which can be done remotely. If your employer refuses either of these options, and you do not feel safe going into work you should take advice. Employmentsolicitor.com says that you could be able to argue for a medical suspension on full pay, which will allow you to stay at home.
Living with someone who is vulnerable or especially at risk is not necessarily a reason an employee can refuse to return to work, says Rycroft. “However, you can, as an employee raise a grievance and ask to be listened to and hopefully a compromise may be agreed, such as unpaid leave or using up annual holiday. But if an employer can show that a workplace is safe, the employer may insist on an employee attending.”
What if I have childcare to worry about?
Legally, you can take time off to look after any dependants – these could be children, or older relatives. This time is typically unpaid. If you are currently furloughed and your employer does not have enough work for everyone to go back full-time, they may agree to leave you on furlough so you can continue to earn 80% of your normal pay.
What information should they give me in advance?
Rycroft says there is no law saying that employers should provide information before you return, but the government guidance to employers recommends that they do. He says this information – written or verbal – should cover how they are making your workplace safe in light of the pandemic. So you should be told what is happening to ensure social distancing and hygiene. “This will allow employees to understand how their health and safety at work is being addressed.
Can I refuse to go back?
Yes, if you believe there is a real danger to going to work. “If an employee refuses to return to the workplace due to the employee reasonably believing imminent and serious danger and is then dismissed for that reason the employee could, depending on the circumstances, have a claim for unfair dismissal,” Gingell says.
“The requirement that the employee has to believe that there is imminent and serious danger, does limit the right.”
Otherwise, you cannot refuse. “If someone refuses to attend work without a valid reason, it could result in disciplinary action,” says Acas. But you may be able to make other arrangements with your employer – perhaps you can use holiday or take unpaid leave, or if you have concerns about something like travelling at peak time, they may be willing to accommodate different shifts. Your employer does not have to agree to this, but it is worth asking.
What if I am worried when I see my workplace?
Rycroft says that under section 100 of the Employment Rights Act 1996 employees may leave a place of work where there is an imminent health and safety danger. So if, for example, you return to find social distancing is impossible, you could argue that this is a reason to leave your workplace.
But in the first instance you should try to resolve the issue with your boss. Gingell says: “Employers ought to to listen to the concerns of individuals and be sympathetic and understanding.”
If you do not get anywhere with this, you should take advice. If you are in a union, it should have a helpline you can call if there is no rep to speak to on site. Acas is another port of call, as is Citizens Advice.
“If the employer has breached the implied obligation to provide a safe working environment and/or trust and confidence an employee could, again, depending on the circumstances, resign swiftly as a result and claim constructive unfair dismissal,” says Gingell. But he says you should get advice before taking this action.
“Another option for employees to consider is contactIng the Health and Safety Executive, which enforces health and safety legislation,” he says.
Friday, 10 April 2020
Information can make you sick
As coronavirus infection rates peak in many countries, the markets rally. There is a nagging worry that a second wave of infections might occur once lockdowns are lifted or summer passes. But for anyone immersed in the financial markets there should be a further concern. Volatility created by the pandemic could itself cause a second wave of health problems. Volatility can make you sick, just as a virus can.
To get an inkling of what this other second wave might look like, it helps to recall what happened after the credit crisis. That event was both a financial and medical disaster. Various epidemiological studies suggest it may be responsible for 260,000 cancer deaths in OECD countries; a 17.8 per cent increase in the Greek mortality rate between 2010-16; and a spike in cardiovascular disease in London for the years 2008-09, with an additional 2,000 deaths due to heart attacks. The current economic crisis may be far worse than 2008-09, so the medical fallout could be as well.
Why do financial and medical crises go hand in hand? Many of the above studies focused on unemployment and reduced access to healthcare as causes of the adverse health outcomes. But research my colleagues and I have conducted on trading floors for the past 12 years suggest to me that uncertainty itself, regardless of outcome, can have independent and profound effects on physiology and health.
Our studies were designed initially to test a hunch I had while running a trading desk for Deutsche Bank, that the rollercoaster of physical sensations a person experiences while immersed in the markets alters their risk-taking. After retraining in neuroscience and physiology at Cambridge University, I set up shop on various hedge fund and asset manager trading floors, along with colleagues, mostly medical researchers. Using wearable tech and sampling biochemistry, we tracked the traders’ cardiovascular, endocrine and immune systems.
My goal was to demonstrate how these physiological changes altered trader performance. Increasingly, though, I came to see that a trading floor provides an elegant model for studying occupational health.
One remarkable thing we found was that traders’ bodies calibrated sensitively to market volatility. For humans, apparently, information is physical. You do not process information dispassionately, as a computer does; rather your brain quietly figures out what movement might ensue from the information, and prepares your body, altering heart rate, adrenaline levels, immune activation and so on.
Your brain did not evolve to support Platonic thought; it evolved to process movement. Our larger brain controls a more sophisticated set of muscles, giving us an ability to learn new movements unmatched by any other animal — or robot — on the planet. If you want to understand yourself, fellow humans, even the markets, put movement at the very core of what we are.
Essential to our exquisite motor control is an equally advanced system of fuel injection, one that has been misleadingly termed “the stress response”. Stress connotes something nasty but the stress response is nothing more sinister than a metabolic preparation for movement. Cortisol, the main stress molecule, inhibits bodily systems not needed during movement, such as digestion and reproduction, and marshals glucose and free fatty acids as fuel for our cells.
The stress response evolved to be short lived, acutely activated for only a few hours or days. Yet during a crisis such as the current one, you can activate the stress response for weeks and months at a time. Then an acute stress response morphs into a chronic one. Your digestive system is inhibited so you become susceptible to gastrointestinal disorders; blood pressure increases so you are prone to hypertension; fatty acids and glucose circulate in your blood but are not used, because you are stuck at home, so your risks increase for cardiovascular disease. Finally, by inhibiting parts of the immune system, stress impairs your ability to recover from diseases such as cancer, and Covid-19.
So why the connection with uncertainty? The stress response is largely predictive rather than reactive. Just as we try to predict the future location of a tennis ball, so too we predict our metabolic needs. When we encounter situations of novelty and uncertainty, we do not know what to expect, so we marshal a preparatory stress response. The stress response is comparable to revving your engine at a yellow light. Situations of novelty can be described, following Claude Shannon, inventor of information theory, as “information rich”. Conveniently, informational load in the financial markets can be measured by the level of volatility: the more Shannon information flowing into the markets, the higher the volatility.
In two of our studies we found that traders’ cortisol levels did in fact track bond volatility almost tick for tick. It did not even matter if the traders were making or losing money; just put a human in the presence of information and their metabolism calibrates to it. Take a moment to contemplate that curious result — there are molecules in your blood that track the amount of information you process.
Today, with historically elevated volatility, there is a good chance cortisol levels are trending higher. Immune systems could also be affected. When your body is attacked by a pathogen, your immune system coordinates a suite of changes known as “sickness behaviour”. You develop a fever, lose your appetite and withdraw socially. You also experience increased risk aversion.
Central to the immune response is inflammation, the process of eliminating pathogens and initiating tissue repair. However, inflammation can also occur in stressful situations, because cytokines, the molecules triggering inflammation, assist in the recruitment of metabolic reserves. If inflammation becomes systemic and chronic, it contributes to a wide range of health problems. We found that interleukin-1-beta, the first responder of inflammation, tracked volatility as closely as cortisol.
Recently we have focused on the cardiovascular system. Working with a large and sophisticated fund manager, we have used cutting-edge wearable tech that permits portfolio managers to track their cardiovascular data, physical activity and sleep. The cardiovascular system similarly tracks volatility and risk appetite.
In short, here we may have a mechanism connecting financial and health crises. On the one hand, fluctuating levels of stress and inflammation affect risk-taking. In a lab-based study, we found that chronically elevated cortisol caused a large decrease in risk appetite. Shifting risk presents tricky problems for risk management — and for central banks. Physiology-induced risk aversion can feed a bear market, morphing it into a crash so dangerous that the state has to step in with asset purchases. On the other hand, chronically elevated stress and inflammation are known to contribute to a wide range of health problems.
We are not accustomed to combining financial and medical data in this way. But corporate and state health programs should start.
The markets today are living through a period of volatility the likes of which I have never encountered. March was, to put it mildly, information rich. As a result, there is now the very real possibility of a second wave of disease. Viruses can make you sick, but so too can information.
Thursday, 9 April 2020
Who to let die and who to keep alive - On the Nice guidelines
In a pandemic, triage starts long before some of us get sick. A new document issued by the British Medical Association (BMA) has set out guidance to ration treatment if the NHS becomes overwhelmed with coronavirus cases.
The BMA suggests that in cases where ventilators are scarce, those facing poor prognosis could have the life-saving equipment taken away from them – even if their condition is improving – with younger and healthier patients given priority instead.
We are already seeing this play out. Last week, one man tweeted that his brother, who lives in a care home with limited mobility and a cognitive disability, went to hospital with a chest infection but didn’t make “the pandemic-led prioritisation cut”. He died a week later.
Meanwhile, it has been reported that a GP practice in Wales issued “do not resuscitate” (DNR) forms to a small number of patients, ensuring that emergency services would not be called should they contract coronavirus and their symptoms worsen. One adult social care provider has said that three of their services have been contacted by GPs to say that they have deemed the people they support should all be DNR. One woman who has received the form so far is in her 20s.
These stories of disabled and older people being denied care have been emerging for weeks as the virus has struck hospitals around the world, but have generally failed to find attention outside the disability community until now.
The National Institute for Health and Care Excellence (Nice) was forced to make a U-turn last week on their advice for the NHS to deny disabled people treatment, but only after disability groups threatened legal action. Nice had told doctors they should assess patients with conditions such as learning disabilities and autism as scoring high for “frailty” - thereby meeting criteria to be refused treatment - based on the fact they need support with personal care in their day-to-day life.
In a health crisis, it is not only the virus that risks infecting society, but our prejudices. It’s a slippery slope of ethical compromises in a culture and medical system that already struggles to support people with disabilities. Research shows that an estimated 1,200 people with a learning disability die avoidably every year due to poor care, while the terms “learning disabilities” or “Down’s syndrome” have been given as the reason for “Do not resuscitate” orders.
In the coronavirus pandemic, doctors are having to make difficult clinical judgments: would a medical intervention help a patient or does their underlying health condition prevent them from benefiting? Is it better to facilitate a peaceful death rather than administer a futile and distressing treatment?
However, judgments based on the efficacy of treatment are not the same as judgments based on the quality of a disabled person’s life. That might be falsely equating support needs with “frailty”, or adopting a blanket policy that withdraws treatment from a whole group of people rather than basing decisions on each individual’s needs and choices. That isn’t healthcare, it’s discrimination.
These are complex issues and we are in deeply difficult times; medics are risking their own lives for the NHS and will face impossible choices as even oxygen and face pumps run low. But that should not mean abandoning debates around key decisions. Indeed, in an emergency it is more important than ever to question our attitudes and responses.
It is worth considering why the default position is to deny life-saving treatment to some disabled people rather than to ask why a wealthy nation that had months to prepare doesn’t have enough resources in the first place. It is worth considering whether talk of “limited resources” is excusing and normalising the long-held idea that disabled lives are disposable.
In recent days, I have seen disabled people take to social media to list their achievements, as if trying to make the case that they are worth saving. A disabled person who has their ventilator removed during this crisis may have gone on to cure cancer. But then, they may have just been loved. A mum with heart disease who always burns her daughter’s birthday cakes. An accountant born with muscular dystrophy who watches Dr Who every Sunday. Disabled people, like all minorities, are only fully human when we are permitted to be as wonderfully average as anyone else.
Utilitarian calculations over the value of certain people’s lives may appear pragmatic right now, but they cost us a part of ourselves. In the coming days, it is inevitable Britain will lose more lives. We need not lose our humanity too.
Wednesday, 1 April 2020
Now the world faces two pandemics – one medical, one financial
We are feeling the anxiety effects of not one pandemic but two. First, there is the Covid-19 pandemic, which makes us anxious because we, or people we love, anywhere in the world, could soon become gravely ill and even die. And, second, there is a pandemic of anxiety about the economic consequences of the first.
These two pandemics are interrelated but are not the same phenomenon. In the second pandemic, stories of fear have gone viral and we often think of them constantly. The stock market has been dropping like a rock, apparently in response to stories of Covid-19 depleting our lifetime savings unless we take some action. But, unlike Covid-19, the source of our anxiety is that we are unsure what action to take.
It is not good news when two pandemics are at work simultaneously. One can feed the other. Business closures, soaring unemployment, and loss of income fuel financial anxiety, which may, in turn, deter people, desperate for work, from taking adequate precautions against the spread of the disease.
Moreover, it is not good news when two contagions are, indeed, global pandemics. When a drop in demand is confined to one country, the loss is partially spread abroad, while demand for the country’s exports is not diminished much. But this time, that natural safety valve will not work, because the recession threatens nearly all countries.
Many people seem to assume that the financial anxiety is nothing more than a direct byproduct of the Covid-19 crisis – a perfectly logical reaction to the disease pandemic. But anxiety is not perfectly logical. The pandemic of financial anxiety, spreading through panicked reaction to price drops and changing narratives, has a life of its own.
The effects financial anxiety has on the stock market may be mediated by a phenomenon that the psychologist Paul Slovic of the University of Oregon and his colleagues call the “affect heuristic.” When people are emotionally upset because of a tragic event, they react with fear even in circumstances where there is no reason to fear.
In a joint paper with William Goetzmann and Dasol Kim, we found that nearby earthquakes affect people’s judgment of the probability of a 1929- or 1987-size stock market crash. If there was a substantial quake within 30 miles (48km) during the previous 30 days, respondents’ assessment of the probability of a crash was significantly higher. That is the affect heuristic at work.
It might make more sense to expect a stock market drop from a disease pandemic than from a recent earthquake, but maybe not a crash of the magnitude seen recently. If it were widely believed that a treatment could limit the intensity of the Covid-19 pandemic to a matter of months, or even that it would last a year or two, that would suggest the stock market risk is not so great for a long-term investor. One could buy, hold, and wait it out.
But a contagion of financial anxiety works differently than a contagion of disease. It is fuelled in part by people noticing others’ lack of confidence, reflected in price declines, and others’ emotional reaction to the declines. A negative bubble in the stock market occurs when people see prices falling, and, trying to discover why, start amplifying stories that explain the decline. Then, prices fall on subsequent days, and again and again.
Observing successive decreases in stock prices creates a powerful feeling of regret for those who have not sold, together with a fear that one might sell at the bottom. This regret and fear prime people’s interest in both pandemic narratives. Where the market goes from there depends on their nature and evolution.
To see this, consider that the stock market in the US did not crater when, in September-October 1918, the news media first started covering the Spanish flu pandemic that eventually claimed 675,000 US lives (and over 50 million worldwide). Instead, monthly prices in the US market were on an uptrend from September 1918 to July 1919.
Why didn’t the market crash? One likely explanation is that world war one, which was approaching its end after the last major battle, the second battle of the Marne, in July-August 1918, crowded out the influenza story, especially after the armistice in November of that year. The war story was likely more contagious than the flu story.
Another reason is that epidemiology was only in its infancy then. Outbreaks were not as forecastable, and the public did not fully believe experts’ advice, with people’s adherence to social-distancing measures “sloppy”. Moreover, it was generally believed that economic crises were banking crises, and there was no banking crisis in the US, where the Federal Reserve System, established just a few years earlier, in 1913, was widely heralded as eliminating that risk.
But perhaps the most important reason the financial narrative was muted during the 1918 influenza epidemic is that far fewer people owned stocks a century ago, and saving for retirement was not the concern it is today, in part because people didn’t live as long and more routinely depended on family if they did.
This time, of course, is different. We see buyers’ panics at local grocery stores, in contrast to 1918, when wartime shortages were regular occurrences. With the Great Recession just behind us, we certainly are well aware of the possibility of major drops in asset prices. Instead of a tragic world war, this time the US is preoccupied with its own political polarisation, and there are many angry narratives about the federal government’s mishandling of the crisis.
Predicting the stock market at a time like this is hard. To do so well, we would have to predict the direct effects on the economy of the Covid-19 pandemic, as well as all the real and psychological effects of the pandemic of financial anxiety. The two are different but inseparable.


