Thomas Frank in The Guardian

There was a time when the Covid pandemic seemed to confirm so many of our assumptions. It cast down the people we regarded as villains. It raised up those we thought were heroes. It prospered people who could shift easily to working from home even as it problematized the lives of those Trump voters living in the old economy.
Like all plagues, Covid often felt like the hand of God on earth, scourging the people for their sins against higher learning and visibly sorting the righteous from the unmasked wicked. “Respect science,” admonished our yard signs. And lo!, Covid came and forced us to do so, elevating our scientists to the highest seats of social authority, from where they banned assembly, commerce, and all the rest.
We cast blame so innocently in those days. We scolded at will. We knew who was right and we shook our heads to behold those in the wrong playing in their swimming pools and on the beach. It made perfect sense to us that Donald Trump, a politician we despised, could not grasp the situation, that he suggested people inject bleach, and that he was personally responsible for more than one super-spreading event. Reality itself punished leaders like him who refused to bow to expertise. The prestige news media even figured out a way to blame the worst death tolls on a system of organized ignorance they called “populism.”
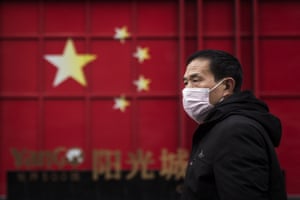
But these days the consensus doesn’t consense quite as well as it used to. Now the media is filled with disturbing stories suggesting that Covid might have come — not from “populism” at all, but from a laboratory screw-up in Wuhan, China. You can feel the moral convulsions beginning as the question sets in: What if science itself is in some way culpable for all this?
*
I am no expert on epidemics. Like everyone else I know, I spent the pandemic doing as I was told. A few months ago I even tried to talk a Fox News viewer out of believing in the lab-leak theory of Covid’s origins. The reason I did that is because the newspapers I read and the TV shows I watched had assured me on many occasions that the lab-leak theory wasn’t true, that it was a racist conspiracy theory, that only deluded Trumpists believed it, that it got infinite pants-on-fire ratings from the fact-checkers, and because (despite all my cynicism) I am the sort who has always trusted the mainstream news media.
My own complacency on the matter was dynamited by the lab-leak essay that ran in the Bulletin of the Atomic Scientists earlier this month; a few weeks later everyone from Doctor Fauci to President Biden is acknowledging that the lab-accident hypothesis might have some merit. We don’t know the real answer yet, and we probably will never know, but this is the moment to anticipate what such a finding might ultimately mean. What if this crazy story turns out to be true?
The answer is that this is the kind of thing that could obliterate the faith of millions. The last global disaster, the financial crisis of 2008, smashed people’s trust in the institutions of capitalism, in the myths of free trade and the New Economy, and eventually in the elites who ran both American political parties.
In the years since (and for complicated reasons), liberal leaders have labored to remake themselves into defenders of professional rectitude and established legitimacy in nearly every field. In reaction to the fool Trump, liberalism made a sort of cult out of science, expertise, the university system, executive-branch “norms,” the “intelligence community,” the State Department, NGOs, the legacy news media, and the hierarchy of credentialed achievement in general.
Now here we are in the waning days of Disastrous Global Crisis #2. Covid is of course worse by many orders of magnitude than the mortgage meltdown — it has killed millions and ruined lives and disrupted the world economy far more extensively. Should it turn out that scientists and experts and NGOs, etc. are villains rather than heroes of this story, we may very well see the expert-worshiping values of modern liberalism go up in a fireball of public anger.
Consider the details of the story as we have learned them in the last few weeks:
- Lab leaks happen. They aren’t the result of conspiracies: “a lab accident is an accident,” as Nathan Robinson points out; they happen all the time, in this country and in others, and people die from them.
- There is evidence that the lab in question, which studies bat coronaviruses, may have been conducting what is called “gain of function” research, a dangerous innovation in which diseases are deliberately made more virulent. By the way, right-wingers didn’t dream up “gain of function”: all the cool virologists have been doing it (in this country and in others) even as the squares have been warning against it for years.
- There are strong hints that some of the bat-virus research at the Wuhan lab was funded in part by the American national-medical establishment — which is to say, the lab-leak hypothesis doesn’t implicate China alone.
- There seem to have been astonishing conflicts of interest among the people assigned to get to the bottom of it all, and (as we know from Enron and the housing bubble) conflicts of interest are always what trip up the well-credentialed professionals whom liberals insist we must all heed, honor, and obey.
- The news media, in its zealous policing of the boundaries of the permissible, insisted that Russiagate was ever so true but that the lab-leak hypothesis was false false false, and woe unto anyone who dared disagree. Reporters gulped down whatever line was most flattering to the experts they were quoting and then insisted that it was 100% right and absolutely incontrovertible — that anything else was only unhinged Trumpist folly, that democracy dies when unbelievers get to speak, and so on.
- The social media monopolies actually censored posts about the lab-leak hypothesis. Of course they did! Because we’re at war with misinformation, you know, and people need to be brought back to the true and correct faith — as agreed upon by experts.
“Let us pray, now, for science,” intoned a New York Times columnist back at the beginning of the Covid pandemic. The title of his article laid down the foundational faith of Trump-era liberalism: “Coronavirus is What You Get When You Ignore Science.”
Ten months later, at the end of a scary article about the history of “gain of function” research and its possible role in the still ongoing Covid pandemic, Nicholson Baker wrote as follows: “This may be the great scientific meta-experiment of the 21st century. Could a world full of scientists do all kinds of reckless recombinant things with viral diseases for many years and successfully avoid a serious outbreak? The hypothesis was that, yes, it was doable. The risk was worth taking. There would be no pandemic.”
Except there was. If it does indeed turn out that the lab-leak hypothesis is the right explanation for how it began — that the common people of the world have been forced into a real-life lab experiment, at tremendous cost — there is a moral earthquake on the way.
Because if the hypothesis is right, it will soon start to dawn on people that our mistake was not insufficient reverence for scientists, or inadequate respect for expertise, or not enough censorship on Facebook. It was a failure to think critically about all of the above, to understand that there is no such thing as absolute expertise. Think of all the disasters of recent years: economic neoliberalism, destructive trade policies, the Iraq War, the housing bubble, banks that are “too big to fail,” mortgage-backed securities, the Hillary Clinton campaign of 2016 — all of these disasters brought to you by the total, self-assured unanimity of the highly educated people who are supposed to know what they’re doing, plus the total complacency of the highly educated people who are supposed to be supervising them.
Then again, maybe I am wrong to roll out all this speculation. Maybe the lab-leak hypothesis will be convincingly disproven. I certainly hope it is.
But even if it inches closer to being confirmed, we can guess what the next turn of the narrative will be. It was a “perfect storm,” the experts will say. Who coulda known? And besides (they will say), the origins of the pandemic don’t matter any more. Go back to sleep.