By late December last year, doctors in the central Chinese city of Wuhan were starting to worry about patients quarantined in their hospitals suffering from an unusual type of pneumonia.
As the mystery illness spread in one of China’s major industrial hubs, some tried to warn their colleagues to take extra care at work, because the disease resembled Sars (severe acute respiratory syndrome), the deadly respiratory disease that had killed hundreds of people across the region in 2002-03 after a government cover-up.
One of those who tried to raise the alarm, though only among a few medical school classmates, was a 33-year-old Chinese ophthalmologist, Li Wenliang. Seven people were in isolation at his hospital, he said, and the disease appeared to be a coronavirus, from the same family as Sars.
In early January he was called in by police, reprimanded for “spreading rumours online”, and forced to sign a paper acknowledging his “misdemeanour” and promising not to repeat it.
Many early cases were linked to the city’s Huanan seafood and fresh produce market, which also sold wildlife, suggesting that the first cases were contracted there.

FacebookTwitterPinterest The Wuhan hygiene emergency response team leave the closed Huanan seafood wholesale market on 11 January. Photograph: Noel Celis/AFP via Getty Images
Scientists would discover the disease had probably originated in bats and had then passed through a second species – in all likelihood, but not certainly, pangolins, a type of scaly anteater – before infecting humans.
But the infections were soon spreading directly between patients, so fast that on 23 January the government announced an unprecedented lockdown of Wuhan city and the surrounding Hubei province.
Two weeks later, on 7 February, Li, who had contracted coronavirus himself, died in hospital from the condition about which he had tried to raise the alarm. He had no known underlying conditions and left behind a wife and young child.
Li became the face of the mysterious new disease. The story of his death and pictures of him in a hospital bed wearing an oxygen mask made media headlines across the globe, including in the UK.
The world, it seemed, was slowly becoming more aware of how lethal coronavirus could be, that it was not just another form of flu with fairly mild symptoms.
But while UK scientists and medical researchers were becoming more concerned, and studying the evidence from China, those among them who were most worried were not getting their messages through to high places.
Distracted by Brexit and reshuffles
The Conservative government of Boris Johnson had other more immediate preoccupations at the start of this year.
Johnson was still basking in his general election success last December. After he returned from a celebratory Caribbean holiday with his fiancee, Carrie Symonds, the political weather for the prime minister seemed to be set fair. It was honeymoon time.
Three and a half years on from the Brexit referendum, the UK was finally about to leave the EU on 31 January. The fireworks and parties for the big night were being planned, the celebratory 50p coins minted.
Minds were certainly not on a developing health emergency far away, as Johnson prepared to exploit the moment of the UK’s departure from the European Union for all it was worth. “I think there was some over-confidence,” admitted one very senior Tory last week.
The prime minister and his chief adviser, Dominic Cummings, wanted to make an early impression at home in other ways too, as domestic reformers. Cummings was waging a war on civil servants in Whitehall, throwing his weight around and deliberately upsetting the Westminster applecart.
While he made the headlines, briefing about his iconoclastic ambitions, Johnson was preparing a big Cabinet reshuffle to assert his own authority in other areas now Brexit was done and dusted.
With Labour effectively leaderless after its fourth consecutive election defeat, there was little opposition to trouble Johnson on any front at all – and certainly no-one of note asking tough questions about coronavirus.
The prime minister duly recast his cabinet team on 13 February – five days after Li’s death in Wuhan. He made big changes but unsurprisingly retained the hitherto safe pair of hands of Matt Hancock as his health secretary.

FacebookTwitterPinterest Boris Johnson speaking about the EU on 3 February. Photograph: Reuters
In a sign of where priorities lay – and the lack of concern that a potential crisis might be heading our way from the east – Hancock wasted no time recording a video of himself grinning with delight on reshuffle day.
He smacked his right fist into his left palm saying he could not wait to “get cracking” and that he relished the chance to deliver the Tories’ manifesto promises, reform social care and improve life sciences. And lastly, in a more sombre voice, he spoke of “dealing with coronavirus and keeping the public safe” before adding, as the grin returned: “Now let’s get back to work!”
It is perhaps too early to conclude for sure that Johnson, Hancock and the government’s entire team of scientific and medical advisers were caught asleep at the wheel. But the fact that Johnson and Hancock themselves, in common with much of the Downing Street staff, would go on to contract the virus or suffer symptoms, further suggests that people at the top had not been sufficiently on their guard.
Now, 11 weeks on from the first cases being confirmed in the UK on 31 January – a period during which more than 14,000 people (and probably several thousands more once care home fatalities are counted) in the UK have died from Covid-19 – and with the country in lockdown, the economy facing prolonged recession as a result, schools closed, and no sign of an end in sight – hard questions have to be asked.
We already know with some certainty that other countries, such as Germany, South Korea, Taiwan and New Zealand, will emerge from this crisis having performed far better than the UK. A few weeks ago the government’s advisers crassly said that fewer than 20,000 deaths would be “a very good result” for the UK.
As we fast approach that grim tally, many experts now believe the UK may come out of this crisis, whenever that may be, with one of the worst records on fighting coronavirus of any European nation. Once the full tally is counted, few expect the number of deaths to be below 20,000.
By contrast, on Friday, Germany was saying it thought it had brought coronavirus largely under control. It had had 3,868 deaths, less a third of the total in the UK (and Germany’s population, at 83 million, is far higher), having conducted widespread testing for Covid-19 from early on, precisely as the UK has failed to do.
How, then, did it come to this? How did coronavirus spread across the globe, prompting different responses in different countries? Did the UK simply fail to heed the warnings? Or did it just decide to take different decisions, while others settled on alternative actions to save lives?
The warnings grow louder
David Nabarro, professor of global health at Imperial College, London, and an envoy for the World Health Organization on Covid-19, says one thing is for sure. All governments were warned how serious the situation was likely to become as early as the end of January. Ignorance of the danger that was coming can be no excuse. Yet it would not be until late March – later than many other countries – that Johnson would announce a complete lockdown.
“WHO had been following the outbreak since the end of December and within a few weeks it called a meeting of its emergency committee to decide if this outbreak was a ‘public health emergency of international concern’,” said Nabarro.
“That is the highest level of alert that WHO can issue, and it issued it on January 30. It made it very clear then – to every country in the world – that we were facing something very serious indeed.”
Well before the end of January, the WHO had been tracking the growing threat minutely: 14 January was a key day in the spread of the disease that would become known as Covid-19. The first case was confirmed outside China, with a woman hospitalised in Thailand.
A WHO official warned then that it was possible that human-to-human transmission had occurred in families of victims – a sign that the disease had potential to spread far and fast – and, inside China, officials were quietly told to prepare for a pandemic.
There was little international attention on the day, though, because Beijing’s dire warnings about a pandemic were made in secret, and a WHO spokesman rowed back from his colleague’s claim.
Officially, China had not seen a new case of the coronavirus for over a week; the outbreak appeared to be fading. It took another six days for China to publicly acknowledge the gravity of the threat, time that scientists believed meant a further 3,000 people were infected.
But on 20 January, officials announced more than 100 new cases and admitted the virus was spreading between humans, a red flag for concern to anyone who works on infectious diseases. The virus could no longer be contained by finding the animal source of the infection and destroying it.
Two days later, the scale of the challenge was made clear to the general public when Beijing locked down millions of people. All transport into and out of the metropolis of Wuhan was cut off, an unprecedented modern quarantine that would come at huge human and economic cost.
On 29 January, the UK would have its first two confirmed cases of the disease. There was little sense that China’s dilemma and its approach – shut down life as we know it or watch the death toll spiral out of control – might have to be our nightmare within weeks.
In early February, Donald Trump announced a ban on travellers who had passed through China in the previous 14 days. Europe began focused testing of people with symptoms and travel histories that linked them to the disease, but little else.
Johnson, it seemed, still had Brexit and free trade much more on his mind. Any hint of draconian action to fight coronavirus that might hurt the economy was the last thing he was entertaining.
In a speech on Brexit in Greenwich on 3 February, he made clear his views on Wuhan-style lockdowns. “We are starting to hear some bizarre autarkic rhetoric,” he said.
”Humanity needs some government somewhere that is willing at least to make the case powerfully for freedom of exchange, some country ready to take off its Clark Kent spectacles and leap into the phone booth and emerge with its cloak flowing as the supercharged champion of the right of the populations of the Earth to buy and sell freely among each other.”
‘Herd immunity’: UK goes it alone
By early March it was abundantly clear to many academics and scientists that the approach being adopted by the UK was markedly different from those followed by other countries. From South Korea to Germany, governments had invested heavily in expanding testing capacity from the first weeks of the epidemic.
Hong Kong, Taiwan and Singapore had brought in controls on travellers from infected regions and strict contact tracing to help understand who could have been exposed, inform them and require self isolation. Face masks became widespread in east Asia, long before it was recommended elsewhere.
Testing and contact tracing has been at the heart of the approach advocated by the WHO, so that countries can establish how transmission chains were occurring, in order to break them.
Many also brought in some social distancing measures, banning large gatherings, closing schools or extending holidays, and encouraged those who could do to work from home. None were as extreme as China’s shutdown, or the European and American lockdowns that would follow.
Writing in the Observer last month, Devi Sridhar, chair of global public health at the University of Ediburgh, noted the distinct UK approach. “Rather than learning from other countries and following the WHO advice, which comes from experts with decades of experience in tackling outbreaks across the world, the UK has decided to follow its own path. This seems to accept that the virus is unstoppable and will probably become an annual, seasonal infection.
“The plan, as explained by the chief science adviser, is to work towards ‘herd immunity’, which is to have the majority of the population contract the virus, develop antibodies and then become immune to it. This theory has been widely used to advocate for mass vaccination for measles, mumps and rubella. The thinking is that, if most of the population is vaccinated, a small percentage can go unvaccinated without cases emerging.”
It was not just the UK whose politicians and scientific advisers were, arguably, slow to act in the early stages. Others countries, including Spain and France, were caught out too, but it was Italy’s tragedy that alerted Europe to the scale of the threat it faced.
European governments and citizens were forced to reckon with the reality that in an age of global travel, the thousands of miles separating them from China meant almost nothing at all. Thousands of Britons were holidaying in Italy the week that it shut down. They were advised to go into self-quarantine on return, but were not registered by the health authorities, nor were their contacts tracked.
Italy and the UK had both had had their first case a day apart at the end of January, but cases rose faster in Italy. The country may just have been unlucky that carriers of the disease flew to its northern cities and ski resorts rather than to other European capitals.
Whatever the reason, cases and then deaths started climbing sharply in northern Italy in late February. Dozens of towns were locked down from the 21st, but in the rest of the country life carried on as normal.
It was soon clear that the problem had not been contained. On 8 March, the prime minister, Guiseppe Conti, quarantined 16 million people across the north of the country, and the next day extended the lockdown to all of Italy.

FacebookTwitterPinterest Russian biological warfare troops, called in by the Italian authorities, disinfect the Pope John Paul I care home near Bergamo. Photograph: Russian Defence Ministry/TASS
The measures saved lives, but came too late for thousands of Italians. The death toll outstripped China, and the world looked on horrified as hospitals were overwhelmed, doctors forced to choose who should have a chance on a ventilator and who should die. On 11 March, the WHO declared a global pandemic. On 14 March, Spain went into lockdown, and three days later France did the same.
But in the UK there appeared to be greater reluctance to act decisively with lockdowns: the banning of mass gatherings and the closure of pubs and restaurants. The government’s scientific and behavioural science advisers were warning ministers that the public might react badly to draconian measures and would not tolerate them for long.
In an apparent show of defiance against the lockdowners, Johnson and Symonds attended the England v Ireland rugby match at Twickenham on 7 March. The Cheltenham Festival, attended over three days to 13 March by 250,000 racegoers, was allowed to go ahead.
Shutdown: Johnson changes tack
The tone was about to change. In a Downing Street press conference on 12 March, Johnson, who had said a few days before the first UK death that the disease was “likely to spread a bit more” suddenly became the deliverer of grave warnings.
Previous talk by his advisers of avoiding lockdowns and developing “herd immunity” had been banished and replaced by a brutal honesty. “I must level with you,” Johnson told reporters. “More families, many more families, are going to lose loved ones before their time.” On 18 March – just days after Downing Street had suggested it was not on the cards – the government announced the closure of all schools until further noticed. Pubs and restaurants were ordered to shut on 20 March. The UK had come late into line.
One former cabinet minister last week described the change of approach as a “screeching U-turn”. Johnson and his ministers were now, even more than before, taking cover behind, and advice from, their scientific and medical advisers. Many of these advisers had become increasingly concerned that the UK had become out of step with other countries because of political resistance from ministers to measures that would hit the economy. The Observer has been told that at least two senior government advisers were on the brink of of quitting before Johnson switched his approach.
The government has found itself unable to escape the consequences of a wider failure to prepare. As hospitals threatened to be overwhelmed before orders were given to massively expand capacity, ministers came under intense criticism over the lack of protective equipment for frontline NHS staff, over the lack of ventilators for patients in intensive care, and for a failure to test more widely for Covid-19, particularly among NHS workers.
The lack of preparedness and instances of chaotic planning has shocked many in and outside the NHS.
Last week, Dr Alison Pittard, the dean of the Faculty of Intensive Care Medicine, the professional body for intensive care practitioners, said the minimum specifications for the government’s own homegrown ventilator scheme would produce machines that would only treat patients “for a few hours”. “If we had been told that that was the case… we’d have said: ‘Don’t bother, you’re wasting your time. That’s of no use’,” she told the Financial Times.
Last month the government missed an EU procurement deadline for ventilators because, minister said, an email went unnoticed. The NHS had said 30,000 more would be needed, Hancock reduced this to 18,000. Pittard said her faculty had been warning for years about a shortage of intensive care capacity and intensive care nurses in hospitals.

FacebookTwitterPinterest Boris Johnson and partner Carrie Symonds with the England captain Owen Farrell at Twickenham on 7 March. Photograph: Facundo Arrizabalaga/EPA
Normally each intensive care patient would have one intensive care nurse in attendance all the time, she said. Now there was one nurse to six patients, although other staff had been redeployed to intensive care units to plug the gaps and the new system was working because of heroic efforts. Although she was reluctant to criticise the government, she said that if the faculty had been listened to, “we wouldn’t be starting from this place”. Germany, she pointed out, has 29 intensive care beds per 100,000 people, compared with six in the UK.
The Tory MP and former health minister Dan Poulter, who works part-time in the NHS, said that given the enormity of the challenge facing government “it almost seems wrong to be critical”.
But he believes part of the problem is that insufficient advice has been sought from experienced NHS clinicians who would have warned of problems with PPE early on, of the shortage of ventilators and would have told ministers of the urgent need to test NHS staff.
“An early over-reliance on academic modelling also resulted in a lack of experienced frontline NHS clinicians – in other words, the people who really understand the day-to-day challenges our hospitals and health service face – from feeding into the initial Covid-19 action plan,” he said. “This has manifested itself amongst other things in the slowness of providing adequate PPE for frontline NHS staff and in the lack of virus testing for healthcare staff in the earlier part of the outbreak.”
How the scientists reacted
When the investigations into the UK’s response to Covid-19 come to be written, there is widespread recognition among experts that this lack of long-term strategic planning will be at the centre of it. So too should be the need to ensure that the views of experts are fed into government more efficiently and widely. The prospect of a previously unknown disease spreading catastrophically around the globe and infecting millions is, after all, not a new one.
Indeed, many warnings have been given in the past about the viral dangers facing humanity. “Given the continual emergence of new pathogens ... and the ever-increasing connectedness of our world, there is a significant probability that a large and lethal pandemic will occur in our lifetime,” Bill Gates predicted several years ago. “And it will have the impact of a nuclear war,” he warned, while urging nations to start stockpiling antiviral drugs and therapies. If only.
For its part, the WHO prepared – several years ago – a list of viruses with no known treatments or vaccines, illnesses that could one day trigger that pandemic and kill hundreds of thousands. Prospective killers included nipah disease and lassa fever as well as an ailment it simply called “disease X” – “a serious international epidemic caused by a pathogen currently unknown”.
As to the most likely nature of that mysterious virus, most modelling assumed that disease X would be flu-like in behaviour, says Dr Josie Golding, the epidemics lead at the Wellcome Trust. After all, influenza had caused so many deadly global outbreaks in the past. As a result, a lot of investment went into making influenza vaccines in preparation, she says. “But have we been thinking about diseases other than influenza that might become pandemics? I don’t think we have. There has been a real gap in our thinking.”
Then came the appearance of Covid-19 – caused not by a strain of influenza but by a coronavirus – in November. Initially, only a few cases were highlighted, a trend that began to change early this year with a rise in numbers of infected ill people.
“The report that really grabbed my attention came out in mid-January,” says epidemiologist Professor Mark Woolhouse at Edinburgh University. “It said 41 cases of this new respiratory illness had now been diagnosed in one small area of China, around Wuhan. And that set the alarm bells ringing for me.”
For Woolhouse, the cluster of cases in one place showed this was not a matter of a few people scattered around China picking up an occasional infection from an animal such as a bat or a chicken. “Forty-one cases in one small area at the same time could not be explained that way. People are not picking this up from animals, I realised. They are actually spreading it to each other. It was already heading out of control.”
Ewan Birney, head of the European Bioinfomatics Institute in Cambridgeshire, also noted the significance of the new disease at the time. “I presumed, at first, that this one would also burn itself out, probably somewhere in Asia,” he says.
His reasoning was straightforward. The outbreak of Sars that appeared in 2003 in China was caused by a coronavirus and killed more than 10% of those it infected. “In fact, it killed or hospitalised so many of those it infected the chain of transmission from one person to others was cut. It was too lethal for its own good. So I thought this might happen with this new disease. But it turns out Covid-19 is much milder and incapacitates fewer individuals, so there is no cut in its transmission. When that became apparent – around mid-January – I became very worried.”
Then there was the infectiousness of the new virus. A person with Sars generally starts to display symptoms before they infect other people. That makes it much easier to contain. But this was not the case with Covid-19. Early data from China – again released in January – showed the virus was being spread from people who were displaying only the mildest symptoms, or in some cases no symptoms. This was making the condition very difficult to track, says virologist Professor Jonathan Ball of Nottingham University.

FacebookTwitterPinterest The County Oak Medical Centre in Brighton was closed on 10 February after a member of staff was infected with coronavirus. Photograph: Glyn Kirk/AFP via Getty Images
“At that point I realised this outbreak was going to be very serious,” he added. “I sent a tweet to a colleague in Australia. It simply said: ‘This one is out of the bag properly’. He sent one back agreeing with me.”
Around this time, Paul Nurse, Nobel laureate and head of the Francis Crick Institute, recalls attending a conference where he met Mark Wolpert, head of UK Research and Innovation, the organisation that funds a vast slice of British scientific research.
“He had just received a text message from a colleague about the outbreak and we started to discuss the implications,” Nurse recalls. “It did not take us long for us both to realise this was going to be very significant. It took another two or three weeks to confirm these worst fears – by mid-February.”
By this time, Birney had realised the virus had a real sting in its tail and could cause serious illness among the elderly and those with other underlying serious ailments. “It was half-term and I was on holiday with my parents. All I wanted to do was to get the holiday over and then get them back to their house in the country where they could keep themselves isolated.”
In February, sporadic cases of Covid-19 were appearing round the country, recalls Tom Wingfield, a clinician and infectious disease expert based at the Liverpool School of Tropical Medicine. “These were cases that had been brought into the country, mainly from China or Italy. Then there was an outbreak in Brighton and I realised that the virus had established itself in a community there. It was a turning point.”
Britain was still doing quite well in containing the disease by testing, tracing contact and setting up quarantine for those suspected of being infected with Covid-19 at this time. “Then, in March, the government decided to abandon this approach and shift from containing the disease to delaying its progress,” says Wingfield. “I would really like to know why the decision to give up testing and contact tracing was taken.”
Many other researchers also question why the government took so long to react to their warnings. “Part of the trouble was there were other virologists who were saying this was going to be like Sars or flu and there was not too much to worry about,” says Ball. “But Sars happened in 2003. The world is much more connected now than it was then. More to the point, Covid-19 was also much more infectious than Sars. And so it started appearing in lots of other countries.
“Perhaps some of us should have got up in front of BBC News and said you lot ought to be petrified because this is going to be a pandemic that will kill hundreds of thousands of people,” adds Ball. “None of us thought this was a particularly constructive thing to do, but maybe with hindsight we should have. If there had been more voices, maybe politicians would have taken this a bit more seriously.”
“There is no question that we were insufficiently prepared,” Nurse says. “We had been warned a few years ago when reports made it clear that the UK was not ready to combat a major flu pandemic and we did not take up that warning. As a result, we were caught out.”
He and many others say an inquiry into Britain’s Covid-19 preparedness will have to be held at some point but stress that this should not be started until the crisis has been dealt with in the UK.
Professor Ian Boyd, a former chief scientific adviser at the Department for Environment, Food and Rural Affairs, agrees. “There is a great danger there will be a lot of looking back with the benefits of hindsight and poking fingers of blame,” warns Boyd. “But when you are in the middle of things you have to make a lot of very hard 50-50 decisions, and sometimes you make the wrong call. On the other hand, there is no harm in making sure that we learn as many lessons as we can.”
The lessons from the rest of the world …
Boris Johnson, after his own brush with death at the hands of Covid-19, will presumably no longer take the gung-ho attitude to illness that he has always has. A former Tory minister said: “If Boris had any sense he would take control of the inquiry and lead it.”
One conclusion that experts are already drawing is that it was those countries close to China, with memories of Sars, or cultural ties to their neighbour, which were much faster to act in response to Covid-19. Perhaps most notable in its success was Taiwan. Closely linked by economic and cultural ties to mainland China, Taiwan could have been at high risk of a major Covid-19 epidemic. Tourists and business people travelled regularly back and forth.
But helped perhaps by having an epidemiologist as vice-president, the government set up a gold standard regime of testing and contact tracing that means that nearly three months on from its first confirmed infection, it has registered fewer than 400 cases and six deaths.
Taiwan’s extensive testing and thorough contact tracing are precisely the kind of action that the former health secretary Jeremy Hunt is demanding before the UK lockdown is lifted. Hunt points out that it is one of the essential conditions set by the WHO to avoid a second wave resulting from an easing of restrictions.
Hong Kong, which also suffered from the Sars crisis, also moved early to enforce quarantine and social distancing, as well as widespread mask wearing, and today has registered just over 1,000 cases and only four deaths.
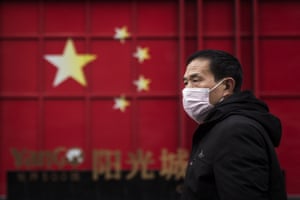
FacebookTwitterPinterest A man in Wuhan on 10 February, the 19th day of the transport lockdown. Photograph: Getty Images
In late February, South Korea looked like it was on a trajectory to disaster, with the highest number of confirmed cases outside China, and numbers rising rapidly. But after the country’s first infection, the government met medical companies and urged them to start developing coronavirus test kits on a massive scale.
The results were impressive. When the epidemic hit, it was ready to deploy largescale testing. Its measures allowed South Korea to become the second country to flatten its coronavirus curve, without the sweeping shutdowns of society and economic activity that China had pioneered and the west would be forced to adopt.
China’s experience should have provided a grim template for western countries to use to prepare. The speed with which Wuhan’s crisis had intensified showed that a relatively advanced medical system could be swamped. Within three weeks there were over 64,000 people infected and 1,000 dead.
The pleas for help from Wuhan’s residents and doctors were to be echoed by those from Italy a few weeks later, and soon after the UK.
Look back three months, and in China there were not enough tests to work out who had coronavirus, there was not enough protective equipment for medical staff treating patients, and then, soon, tragically there were not enough hospital beds and ventilators for sick patients. These are exactly the challenges faced by authorities from New York to Rome, London to Madrid.
… and the other country that didn’t listen
If the UK has serious questions to answer, the country that so far has seen the worst of the outbreak, the United States, was slowest of all to act. Trump for months ignored, played down or lied about the threat posed by coronavirus, leaving individual states to act unilaterally as it became clear it had already taken hold on US soil.
On 17 March parts of California issued “shelter in place” orders, effectively a lockdown. By the end of that week New York City had also shut down, along with a dozen states, and the majority of the rest of the country had put some restrictions in place. Only five states had few or no controls.
There have now been nearly 700,000 confirmed cases in the US and over 33,000 deaths; actual numbers are likely to be higher for both. The economy has also been devastated, with more than 22 million out of work as businesses collapse or shrink under the strain.

The US was slowest of all to act, but Donald Trump is preparing to lift restrictions already. Photograph: Alex Brandon/AP
Trump insists the US is turning a corner, and has tried to blame – among other targets – the WHO for failing to fully raise the alarm, and has stripped it of its US funding.
There have certainly been questions about the organisation’s strong praise for China and the exclusion of Taiwan, which may have contributed to the delay in recognising human-to-human transmission was occurring. But it began daily briefings on 22 January and had declared a global health emergency by the end of that month.
While initially sceptical about China’s distancing measures, it urged other countries to adopt them once there was evidence they were working. It warned about shortages of PPE over a month ago, and since the beginning of the outbreak has urged countries, including the UK, to “test, test, test” to contain the virus – a strategy followed by almost all countries that have managed to suppress it.
A senior Whitehall source with detailed knowledge of the UK’s response and those of other countries said: “The fact is that those countries who knew a lot about Sars quickly saw the danger. But in the UK the attitude among politicians and also scientists was that it was really just some form of a flu. All the government’s pandemic planning was based on a flu scenario. And then it turned out to be something different and far, far worse and the response was completely inadequate.”
And we are going to be living with the consequences for a long time. Don’t expect a vaccine to come to the rescue in the short term, says Nabarro. “For the foreseeable future, we are going to have to find ways to go about our lives with this virus as a constant threat to our lives. That means isolating those who show signs of the disease and also their contacts. Older people will have to be protected. That is going to be the new normal for us all.”