'People will forgive you for being wrong, but they will never forgive you for being right - especially if events prove you right while proving them wrong.' Thomas Sowell
Search This Blog
Showing posts with label hospital. Show all posts
Showing posts with label hospital. Show all posts
Wednesday, 20 September 2023
Saturday, 15 April 2023
Sunday, 23 May 2021
Monday, 13 April 2015
Hospital patients to be asked about UK residence status
BBC News
Patients could be made to show their passports when they use hospital care in England under new rules introduced by the Department of Health.
Those accessing new treatment will be asked questions about their residence status in the UK.
Patients may need to submit passports and immigration documents when this is in doubt, the department said.
Hospitals will also be able to charge short-term visitors from outside Europe 150% of the cost of treatment.
The department said the new rules came into force on 6 April for overseas visitors and migrants who use NHS hospital care in England.
Primary care and A&E care will remain free.
There will also be financial sanctions for trusts which fail to identify and bill patients who should be charged, it said.
The plans are part of a crackdown on so-called "health tourism".
Andrew Bridgen, the Tory MP for North West Leicestershire in the last Parliament,told the Daily Mail: "This is not the International Health Service, it's the National Health Service.
"Non-UK nationals seeking medical attention should pay for their treatment.
"The NHS is funded by UK taxpayers for UK citizens and if any of us went to any of these countries we'd certainly be paying if we needed to be treated."
Most foreign migrants and overseas visitors can currently get free NHS care immediately or soon after arrival in the UK but they are expected to repay the cost of most procedures afterwards.
The charges are based on the standard tariff for a range of procedures, ranging from about £1,860 for cataract surgery to about £8,570 for a hip replacement.
Non-UK citizens who are lawfully entitled to reside in the UK and usually live in the country will be entitled to free NHS care as they are now.
Patients could be made to show their passports when they use hospital care in England under new rules introduced by the Department of Health.
Those accessing new treatment will be asked questions about their residence status in the UK.
Patients may need to submit passports and immigration documents when this is in doubt, the department said.
Hospitals will also be able to charge short-term visitors from outside Europe 150% of the cost of treatment.
-----Also read
UK TOURISTS BEWARE – Cambridge Hospital Staff Demand Instant Money from Sick and Ailing Indian Tourist
-------
The department said the new rules came into force on 6 April for overseas visitors and migrants who use NHS hospital care in England.
Primary care and A&E care will remain free.
There will also be financial sanctions for trusts which fail to identify and bill patients who should be charged, it said.
The plans are part of a crackdown on so-called "health tourism".
Andrew Bridgen, the Tory MP for North West Leicestershire in the last Parliament,told the Daily Mail: "This is not the International Health Service, it's the National Health Service.
"Non-UK nationals seeking medical attention should pay for their treatment.
"The NHS is funded by UK taxpayers for UK citizens and if any of us went to any of these countries we'd certainly be paying if we needed to be treated."
Most foreign migrants and overseas visitors can currently get free NHS care immediately or soon after arrival in the UK but they are expected to repay the cost of most procedures afterwards.
The charges are based on the standard tariff for a range of procedures, ranging from about £1,860 for cataract surgery to about £8,570 for a hip replacement.
Non-UK citizens who are lawfully entitled to reside in the UK and usually live in the country will be entitled to free NHS care as they are now.
Monday, 2 February 2015
Depression and spiritual awakening -- two sides of one door
Depression and spiritual awakening -- two sides of one door Lisa Miller
Lessons from the Mental Hospital -- Glennon Doyle Melton
Psychosis or Spiritual Awakening
Sunday, 9 March 2014
On the NHS frontline: 'being a doctor in A&E is like being a medic in a war zone'
Doctor explains why she decided to make a film depicting the real-life drama of targets and staff pushed to the limit
The start of a shift and I brace myself as I walk into the waiting area. A huge number of people are already there, waiting to be called. I try to avoid eye contact. It's like entering an arena but I feel more like the sacrificial lamb than a gladiator. Entering the main area of the emergency department, a scene of chaos. All available space to see patients is occupied. Staff shout instructions to each other above the noise. I hear a patient vomiting, another is crying out in pain and an elderly woman's voice cuts through, confused and repeating that she wants to go home. "So do I," I whisper to myself.
Colleagues run between cubicles with clean sheets, urine pots and trays for taking blood. Ambulance sirens heard above the noise signal that more patients are coming. A cardiac arrest case is sped into the resuscitation room with paramedics pumping the chest of a patient as the rest of the crash team run through. The atmosphere is explosive and adrenaline charged.
A senior doctor in the middle of the storm tries to bring order in a place that refuses to be controlled. Junior doctors are flushed, red in the face, eyes wide with a hint of panic. I find a tearful one at the computer. She is new and hating every second of it. There isn't time or even space to console her with a pep talk. Give her a few more weeks and the hard outer shell will develop like body armour.
My first patient of the shift needs a full neurological exam. I hunt around for a pen torch to shine into her eyes. "Make sure you have your weapons before you go to war," says a fellow registrar, wryly, handing over the torch. I smile. This is not Palestine, Libya or Syria. This is a hospital on the eastern outskirts of London.
 The A&E department at Queen's hospital in Romford deals with 400 patients a day.
The A&E department at Queen's hospital in Romford deals with 400 patients a day.
Being a doctor in accident and emergency has at times resembled being a medic in a war zone. I have worked as a doctor in various conflicts and yet some of my most stressful moments, facing a tidal wave of pressure, have happened closer to home, in Queen's hospital, Romford.
The UK's A&E departments have been described by the College of Emergency Medicine (CEM) as facing a crisis. The term was specifically chosen to describe the situation that everyone from the most senior consultant to the most junior nurse is experiencing. Last year Dr Cliff Mann, the CEM president, wrote in a press release: "A lack of a plan for resolution [is] an existential threat to emergency medicine."
There are recurrent themes causing the crisis: more people are coming to A&E; a falling number of doctors want to work there because of the pressures involved and the poor work/life balance; and hospitals are increasingly full – resulting in bottlenecks that back up into the emergency department.
Over the past four progressively worse winters I came to a tipping point. Nothing in the media was reflecting the daily realities of being a doctor on the shop floor. Last April, when the CEM's press release hit the headlines, I took my cue.
I divide my time as an A&E doctor and film-maker. I wanted to make something honest and reflective of the reality.
After a year's worth of access negotiation, I began filming with the Guardian this winter in two hospitals – Queen's where I work as a middle-grade locum, and Musgrove Park, in Taunton, Somerset, where Cliff Mann also works.
"For a long time we were like John the Baptist, crying into the wilderness and no one was listening," Mann said to me, while on shift at Musgrove Park. The most senior consultant within emergency medicine leads from the front, including a Friday shift that runs from 3pm to midnight. "No one goes into emergency medicine thinking it's going to be easy and calm – that would be bizarre. But if you push the individual with persistently increasing intensity levels they will start to fade."
The TV stories of George Clooney and the ER cast don't come close to reality. My research into the speciality obviously went beyond watching medical dramas but nothing prepared me for what it was actually like.
Attending conferences in emergency medicine becomes almost therapeutic in its sharing of experiences. At an emergency medicine conference, Expanding Scientific Horizons, held in Twickenham, south-west London, last year, it was telling that the sessions entitled Creating Satisfaction and Maintaining Wellbeing in Emergency Medicine were standing room only.
One of the speakers, Susie Hewitt, a consultant from Derby, spoke about her battle with depression during the time she was appointed head of service for the introduction of the four-hour target – the government's instruction that 95% of patients should be seen within four hours of arriving at A&E.
The culmination of work and personal pressures resulted in what Hewitt describes as being "hit with what felt like a big freight train".
Many of us recognised ourselves in that. At the conference leaflets for well-being support and therapies were being distributed widely. We are clearly not a very healthy bunch right now.
The CEM warned the government three years ago that there was a problem with falling numbers of staff, but no concrete solutions emerged. I began to see my own consultants and middle-grade colleagues make plans to fly to the other side of the world.
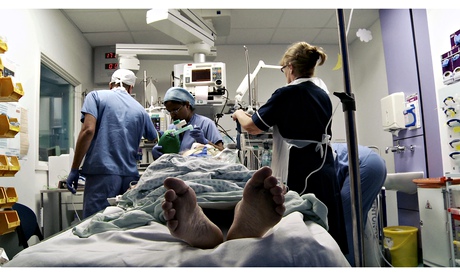 Medics with a patient at Queen's hospital. The hospital was built for 90,000 patients a year but receives 140,000.
Medics with a patient at Queen's hospital. The hospital was built for 90,000 patients a year but receives 140,000.
Queen's A&E, part of the Barking, Havering and Redbridge University Trust, sees about 400 patients a day and its sister hospital, King George's, sees 200. The trust serves a population of 750,000 and is one of the UK's largest. It also has one of the highest elderly populations in London. Following a report by the Care Quality Commission (CQC) that its A&E was "at times unsafe because of the lack of full-time consultants and middle-grade doctors", Queen's became the 14th hospital to be put into special measures last December. Filming with the Guardian inside its A&E began the next day.
The hospital was built for 90,000 patients a year but receives 140,000. Ironically, King George's A&E, which performs better against targets, is scheduled for closure in 2015, after a unanimous vote by local primary care trusts. Queen's is expected to absorb the extra numbers. Queen's is understaffed, with only eight full-time consultants where it requires 21 in order to provide 24-hour cover, seven days a week. Four consultants left last year.
One of them, Dr Rosie Furse, described the pressure of targets. Battles with certain specialities to accept patients on to their wards are also a common complaint. She left for a post on the island of Mustique before being recruited to a hospital in Bath.
David Prior, chairman of the CQC, was reported in the Guardian in May 2013 as saying too many patients were arriving at hospital as emergency cases, and improved earlier care in the community was needed. He suggested more acute beds should be closed. "Emergency admissions through accident and emergency are out of control in large parts of the country," he said.
That prompted memories of a recent bed-blocked day in Queen's. Matron Mary Feeney rushed into A&E having secured a bed on the intensive therapy unit for an unwell patient in an A&E cubicle.
"They say bring him in half an hour – half an hour we have not got," and with that the patient was out of the door on the way with matron off to negotiate access at the hallowed gates of ITU.
A significant contributor to breaches of the four-hour target is the quest to find a bed for someone who is clearly not well enough to go home. Over Christmas one woman was brought in with diarrhoea and a ruptured bowel requiring a surgical side room. She waited in A&E for 17 hours until a room became available. Another woman was brought in with high blood sugars and needed an acute medical bed. I saw her when she arrived in the evening and then met her the next morning when I came back to work. That's when A&E becomes a ward.
On the first day of filming we had four intubated, unconscious patients in the resuscitation room at the same time, all of them requiring critical beds. The rest of the room was full of acutely unwell patients being redistributed around A&E as more room was needed with each new ambulance arrival.
Finding alternatives to A&E through improved care in the community is essential but if more acute beds close the A&E waits will get longer for sick patients requiring admission.
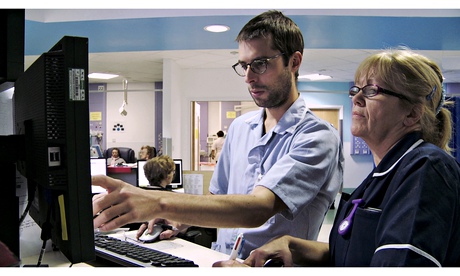 Staff at work at Queen's hospital. The hospital has only eight full-time consultants.
Staff at work at Queen's hospital. The hospital has only eight full-time consultants.
I went through a period of having palpitations during a stretch of extremely challenging shifts last winter. It was when I had a palpitation and nearly passed out while driving that I decided to step down my intensity of work. I had further investigations but the remedy was obvious. I reduced my shifts and the palpitations have stopped.
Over the past three years I have worked harder than in my previous life in the army. I went through the Sandhurst commissioning course, renowned for its tough schedule, but in accident and emergency medicine at its peak, the intensity is tougher.
The CEM published an aptly named report – Stretched to the limit – in October last year. It described a consultant workforce under pressure. As a middle grade I wonder if actually I can physically do the job of a consultant.
The report said: "Evidence confirms that burnout among physicians in emergency medicine occurs at the highest rate of all medical specialities. There is also a very worrying trend developing of consultants seeking to move abroad after having been trained in the NHS."
The report details 21 consultants having left the UK in 2013 with an overall exodus of 78 since 2008.
Within the report details of a survey reveal that consultants on average plan to retire at 60 with the current job not compatible with advancing age. "Doing four nights in a row when you are 50 or 55 is physically impossible," said Dr Antoine Azzi, a specialist registrar working at Queen's at the very end of his training and soon to be a consultant.
He hopes for a less intense workload as a consultant, but it appears that is not going to be the case. The report said that 40% of the consultant workforce were on call one night in every six. The average age of emergency medicine consultants is 43 and the survey showed most plan to retire at 60.
The things that make a difference include access to training, which provides juniors with skills they need and reduces a layer of stress.
Before she left, Furse, like many other consultants, was dedicated to improving the working lives of her trainees and colleagues.
On one occasion I placed a chest drain into a patient with a spontaneous pneumothorax – a collection of air between the lung and the chest wall. If I failed, he could go into respiratory arrest, which could lead to death.
Furse stood by, calm and instructive. "Get it in quick, Saleyha," was all she said. I urged the drain's tube into his chest and the moment I saw the swinging bubble of the drain, signalling a successful placement I allowed myself to breathe and the patient was stabilised.
Moments like that are what makes being a doctor count but opportunities for training are few as workload grows.
The constant turnover of new junior doctors hits the department, too. Most junior doctors who spend six months in A&E leave at the end of their assignment with a lot of experience, but they are relieved to be going and they won't be coming back.
Mann says: "They come and do their six-month attachment and at the end say, "Thank you very much, it was interesting but I am moving on because it nearly killed me.'"
There is a quote from Hippocrates that says: "Where there is a love of medicine, there is a love of humanity." I see this every day to some degree in A&E. Before she left Furse reminded us during a teaching session: "Patients are key to everything we do and if you stop caring about them – well you should not be here any more."
Looking back on diary entries related to shifts I did last year during the spell when I was having palpitations I was reminded why I put myself through it. It's what makes us go back the next day no matter how awful the shift has been.
I wrote: "It was hard, I am tired and I was pushed but I feel alive. Today counted. I cared for patients and they remained the main focus of my day. Nothing else. Patients arrive here to be seen on possibly the worst days of their lives and through them we learn so much about our art. They teach us how to be doctors. As I walked into work today I was hit by reflection of all the patients who have left their mark – the ones that didn't make it.
"They stay with you, like companions. I shared the last few hours of their lives with them … forming a bond that transcends into something almost spiritual even for those that don't believe. Above all else, that is what counts and it remains a privilege."
Thursday, 14 March 2013
Your five worst medical nightmares
From a doctor amputating the wrong leg, to a woman given the wrong baby, hospital treatment does not always go to plan. Luckily, though, mistakes are rare

One unhappy patient … Kenneth Williams in the 1967 film Carry on Doctor. Photograph: ITV/Rex Features
It sounds like a classic nightmare – waking up during an operation to find you can't move. But that's what happened to one patient, Sarah Newton. "I was trying to scream. I tried to wiggle my toes desperately hard but I couldn't move anything." Thankfully, "accidental awareness", as it is known, is rare. A survey from the Royal College of Anaesthetists says it occurs once in every 15,000 operations under general anaesthetic, or 153 times in 2011 – and is usually brief and painless. But what of our other medical terrors?
Wrong site surgery
Usually the cause is a catastrophic series of administrative errors, such as when Dr Rolando Sanchez, a Florida surgeon, was told by a nurse that he was amputating the wrong leg of his patient just as he finished cutting through it. Luckily, with only 70 incidents recorded by the NHS in the year 2011-12, it is extremely unusual.
Wrong patient surgery
Never mind the wrong limb. How about operating on the wrong body? Sometimes there may be a mix-up over two people with the same name. Or similar procedures. The reality may not be as scary as it sounds – recently a patient in Cambridgeshire was given another patient's lens during eye surgery, although this was soon corrected. Plus there were fewer than 10 incidents reported in the UK during 2011-2.
Retained instruments
Leaving surgical instruments inside patients occurred 161 times in 2011-12. Often it's a sponge, which can lead to serious infections. The risk arises in emergency surgery, and in surgery on obese patients, but it is still very unlikely to happen to you.
Baby mix-ups
Despite being a common storyline in films or stories, there are few documented cases of mothers sent home with the wrong baby. But you have to ask: how would they know? In Romania in 2008, Cristina Zahariuc noticed because the daughter she was sent home with turned out to have a penis. Despite a few awful stories, the risk will be lower now that most babies stay with their parents immediately after birth.
Being treated by an impostor
Well, it has happened. In September 2011, 17-year-old Matthew Scheidt was convicted, of impersonating a physician's assistant in Florida. He dressed wounds, attended surgery, examined naked patients and even administered CPR. While New Zealander Richmal Oates-Whitehead treated victims of the 7 July 2005 bombings in London, despite not being medically qualified.
Ferdinand Waldo Demara managed fairly well when he conducted a series of major operations by speed-reading textbooks during the Korean war. And a man called Gerald Barnes even managed to impersonate a doctor, and be convicted of it, five times. Thankfully pretenders do tend to get caught.
Friday, 14 December 2012
Jacintha Saldanha: Duchess hospital nurse suicide note 'criticised hospital'
A suicide note left by the nurse found dead after the hoax call to the hospital treating the Duchess of Cambridge criticised fellow staff, it emerged tonight.
The letter was one of three Jacintha Saldanha, 46, wrote before she was found
hanging in her room at a nurses’ accommodation block at the King Edward VII
Hospital in London last Friday.
Injuries to her wrists were also found, a coroner heard today. Attempts were
made to revive the nurse but they were "to no avail".
Mrs Saldanha, from Bristol, had left three suicide notes for her family and had also written emails and made telephone calls that police believe might help shed light on what happened, the court was told.
Tonight, reports claimed that one note specifically addresses her employers and criticism of hospital staff despite officials previously maintaining they were fully supportive of the nurse.
The Guardian reported that one note also specifically referred to the hoax call made by the two Australian radio presenters while a third detailed wishes for her funeral.
Two notes were found at the scene in central London and the third recovered in
the nurse’s belongings.
The mother of two’s family has been given typed copies of the three handwritten notes by the police and has read the contents, the Guardian claimed.
It has been reported that the family did not know about the hoax call until after Mrs Saldanha’s death.
Today, during a five-minute hearing at Westminster Coroner’s Court, Det Chief Insp James Harman said Mrs Saldanha, a night sister, was found by a colleague and a security guard who called the emergency services.
DCI Harman told the court: “At this time there are no suspicious circumstances apparent to me in relation to this death.”
Detectives are talking to witnesses, friends, colleagues and Mrs Saldanha’s telephone contacts, DCI Harman said, in order to establish the circumstances that may have led to, and contributed, to her death.
Referring to the two 2 Day FM presenters who made the prank call, he added: “You will be aware of the wider circumstances in this case and I can expect in the very near future we will be in contact with colleagues in New South Wales to establish the best means of putting the evidence before you.”
Coroner’s officer Lynda Martindill said Mrs Saldanha’s accountant husband Ben Barboza, 49, had identified her body. The coroner opened and adjourned the inquest, with a full hearing listed for March 26 next year.
None of Mrs Saldanha’s family attended the hearing, but one of her colleagues was there. The coroner said: “Can I express my sympathy to you and to the family.”
Mrs Saldanha was a nurse at King Edward VII hospital, West London, where the Duchess of Cambridge was being treated for severe pregnancy sickness.
During the hoax call, the nurse transferred the DJs, believing they were the Queen and Prince of Wales, to a colleague who described in detail the condition of the Duchess of Cambridge during her hospital treatment for severe pregnancy sickness.
The Australian DJs, Mel Greig and Michael Christian, have both issued emotional apologies for her death and have since been moved into “safe houses” and given 24-hour bodyguards after receiving death threats.
It emerged last night that the broadcasters responsible for airing the call are to be officially investigated by the Australian Communications and Media Authority, which regulates radio broadcasting, in line with the Commercial Radio Codes of Practice.
Her family are set to receive more than £320,000 from Southern Cross Austereo, the parent company for whom the presenters work for.
The hearing comes on the day that Southern Cross Austereo (SCA) is to resume advertising on 2 Day FM. All profits from the adverts until the end of the year will be donated to a memorial fund established in aid of her family.
Keith Vaz, the Labour MP who is helping Mr Barboza, daughter Lisha, 14, and son Junal, 16, said a memorial service would be held in Bristol tomorrow, followed by one in Westminster Cathedral on Saturday. The hospital has offered bereavement counselling for the family in Bristol, which they have decided to take up, he added.
He did not attend the hearing but said of the family: “They are grieving in their homes, they are comforting each other and the community is comforting them, that is why they have not come.” Her body was released to her family in order to arrange her funeral in India.
A hospital spokeswoman tonight said no one in senior management knew what the contents of the notes left were but she said officials “were very clear that there were no disciplinary issues in this matter”.
Both the nurses involved had been offered “full support” and “it was made clear they were victims of a cruel journalistic trick,” she added.
The mother of two’s family has been given typed copies of the three handwritten notes by the police and has read the contents, the Guardian claimed.
It has been reported that the family did not know about the hoax call until after Mrs Saldanha’s death.
Today, during a five-minute hearing at Westminster Coroner’s Court, Det Chief Insp James Harman said Mrs Saldanha, a night sister, was found by a colleague and a security guard who called the emergency services.
DCI Harman told the court: “At this time there are no suspicious circumstances apparent to me in relation to this death.”
Detectives are talking to witnesses, friends, colleagues and Mrs Saldanha’s telephone contacts, DCI Harman said, in order to establish the circumstances that may have led to, and contributed, to her death.
Referring to the two 2 Day FM presenters who made the prank call, he added: “You will be aware of the wider circumstances in this case and I can expect in the very near future we will be in contact with colleagues in New South Wales to establish the best means of putting the evidence before you.”
Coroner’s officer Lynda Martindill said Mrs Saldanha’s accountant husband Ben Barboza, 49, had identified her body. The coroner opened and adjourned the inquest, with a full hearing listed for March 26 next year.
None of Mrs Saldanha’s family attended the hearing, but one of her colleagues was there. The coroner said: “Can I express my sympathy to you and to the family.”
Mrs Saldanha was a nurse at King Edward VII hospital, West London, where the Duchess of Cambridge was being treated for severe pregnancy sickness.
During the hoax call, the nurse transferred the DJs, believing they were the Queen and Prince of Wales, to a colleague who described in detail the condition of the Duchess of Cambridge during her hospital treatment for severe pregnancy sickness.
The Australian DJs, Mel Greig and Michael Christian, have both issued emotional apologies for her death and have since been moved into “safe houses” and given 24-hour bodyguards after receiving death threats.
It emerged last night that the broadcasters responsible for airing the call are to be officially investigated by the Australian Communications and Media Authority, which regulates radio broadcasting, in line with the Commercial Radio Codes of Practice.
Her family are set to receive more than £320,000 from Southern Cross Austereo, the parent company for whom the presenters work for.
The hearing comes on the day that Southern Cross Austereo (SCA) is to resume advertising on 2 Day FM. All profits from the adverts until the end of the year will be donated to a memorial fund established in aid of her family.
Keith Vaz, the Labour MP who is helping Mr Barboza, daughter Lisha, 14, and son Junal, 16, said a memorial service would be held in Bristol tomorrow, followed by one in Westminster Cathedral on Saturday. The hospital has offered bereavement counselling for the family in Bristol, which they have decided to take up, he added.
He did not attend the hearing but said of the family: “They are grieving in their homes, they are comforting each other and the community is comforting them, that is why they have not come.” Her body was released to her family in order to arrange her funeral in India.
A hospital spokeswoman tonight said no one in senior management knew what the contents of the notes left were but she said officials “were very clear that there were no disciplinary issues in this matter”.
Both the nurses involved had been offered “full support” and “it was made clear they were victims of a cruel journalistic trick,” she added.
Friday, 7 December 2012
Morphine: The cheap, effective pain-relief drug denied to millions
By Joanne Silberner PRI's The World
 In the UK and US, patients who
need morphine get it - it's a different story elsewhere
In the UK and US, patients who
need morphine get it - it's a different story elsewhere
It's cheap, effective and easy to
administer - so why are millions of people around the world dying in pain,
without access to morphine?
In an open ward at Mulago Hospital in Uganda's capital city, Kampala, an elderly woman named Joyce lies in the fifth bed on the left.
She has twisted the sheets around herself, her face contorted by pain. Joyce's husband, thin and birdlike, hovers over her.
Joyce has cancer - it has spread throughout her body - and until a few days ago, she was on morphine. Then it ran out.
"She's consistently had pain," says a nurse. "And she describes the pain to be deep - kind of into her bones."
The Ugandan government makes and distributes its own morphine for use in hospitals, but poor management means the supply is erratic.
"We're in a very difficult situation," says Lesley Henson, a British pain specialist on duty at Mulago Hospital. They have patients whose pain has been kept under control with morphine - but they are running out it.

In many ways, morphine is an excellent drug for use in developing countries. It is cheap, effective, and simple and easy to administer by mouth.
Yet according to the World Health Organization, every year more than five million people with cancer die in pain, without access to morphine.
"The fact that what stands between them and the relief of that pain is a drug that costs $2 [£1.25] a week, I think is just really unconscionable," says Meg O'Brien, head of The Global Access to Pain Relief Initiative, a non-profit organisation that advocates for greater access to morphine.
O'Brien says in well-off countries, like the UK and United States, there is enough morphine to treat 100% of people in pain - but in low-income countries, it's just 8%.
In many low- and middle-income countries - 150, by some counts - morphine is all but impossible to get. Some governments don't provide it, or strictly limit it, because of concerns that it will be diverted to produce heroin.
And many doctors are reluctant to prescribe morphine, fearing their patients will become addicted.
In India, whether you can get morphine depends largely on where you are treated.
Tata Memorial Hospital, a modern and well-equipped
medical centre in Mumbai, has no problem getting morphine for patients.
"We have all the medicines necessary," says Dr Mary Ann Muckaden, head of pain relief at the hospital. "We never run out."
But in other parts of the country, it's a different story. Muckaden estimates only 1% to 2% of Indians with cancer pain get morphine.
Dinesh Kumar Yadav, 28, has come to Tata Memorial - a 30-hour bus ride from his home - to get morphine for his wife.
He tells me she is bedridden with pain but can't get morphine in the north Indian state where they live.
Dr Muckaden says part of the problem is a stifling bureaucracy.
"Many physicians in the north, they don't want to go through the rigorous licensing to store morphine," she explains.
A morphine-use map of the world

- $2 (£1.25) - cost per week per patient
- 100% - percentage of people in UK and US who have access to morphine, if they need it
- 8% - percentage in the developing world who get morphine when required
- 20% of the world's painful deaths are in sub-Saharan Africa, but only 1% of morphine use
There is a place in India where there are no barriers to
morphine. But even at the CIPLA Palliative Care Centre in the city of Pune, in
Maharashtra state, there are still challenges.
You don't see the challenges when you walk through the cool courtyard gardens with fountains and manicured walkways, or in the beautiful whitewashed buildings with large airy wards, each named after a flower.
"This is heaven on earth," says Asha Dikshit, whose mother came here last year in the last stages of breast cancer.
"She was in agony. Her shoulder had dislocated. It could not be fixed back," says Dikshit. "She had pain in the back, and sometimes there were hallucinations."
But she says her mother died - peacefully - on morphine.
Making morphine

- Comes from the opium poppy
- Discovered in 1804
- First marketed for pain relief in 1817
- Recommended by WHO for pain relief under certain conditions
Every patient here has cancer, and the care is free. The
Indian generic drug manufacturer CIPLA supplies the morphine and pays all the
other expenses.
But even with all the centre offers, the occupancy rate runs at only about 60%. One big reason, says director Priya Kulkarni, is a result of patients' own concerns about morphine. They often think morphine equals death, and they recoil when doctors suggest it.
Kulkarni says many local oncologists don't want to send patients here for that reason.
"They don't want to give up when it comes to giving them hope," she says. "And saying something like, 'I am going to refer you to a palliative specialist,' is indirectly saying 'There is nothing more I can do for you.'"
Despite all the obstacles to the use of morphine in the developing world, Kulkarni and others say things are starting to move in their direction.
In low-income countries, morphine consumption is up tenfold since 1995, according to the International Narcotics Control Board. And several countries where not many years ago there was no morphine - like Uganda - at least have some today, even if the supply is unreliable.
Back at the hospital in Kampala - where the pharmacy ran out of morphine and Joyce, the cancer patient, had to go without - palliative care specialist Leslie Henson finds a bit of luck. After leaving her patient, she steps into an office, glances at a bookshelf, and sees a forgotten bottle of morphine. It's enough to treat two or three people.
"Hopefully, we'll go take this to her and see what we can do," she says as she troops back to Joyce's room.
Soon, a doctor administers the morphine.
Joyce smiles. Her face untwists. And her husband looks ecstatic.
I ask Joyce if she's glad to get the morphine. Her husband answers. "Very much, indeed."
Other people in the hospital will remain in pain - there is not enough morphine to go around - but for the next few hours, at least, Joyce will be pain-free.
Thursday, 1 September 2011
To all friends who have relatives visiting from outside the UK
You are aware about the way NHS hospitals prey on foreigners who happen to fall ill during their visit to the UK -for details please visit
http://giffenman-miscellania.blogspot.com/2011/08/uk-tourists-beware-cambridge-hospital.html
I have now created an e-petition on the government website which states 'a Visitor's visa fee should include provision of medical insurance to cover emergencies'. It requires signatures of 100, 000 folks resident in the UK for it to be discussed in parliament. This will I hope prevent predatory behaviour from staff at NHS hospitals. Kindly sign this petition if you agree with it. Also please forward it to as many UK residents you know so that the petition reaches the discussion stage in parliament. You can sign the petition here.
http://epetitions.direct.gov.uk/petitions/15381
Thank you
Sunday, 28 August 2011
British Tourism
You have all seen images of the injured Malaysian tourist being robbed by British citizens.
Now VISUALISE THE NEXT SCENE.
This tourist is in an NHS hospital having recovered his consciousness. His hospital bed is now visited by predatory finance staff from the hospital demanding that he produce instant cash or he will be deported.
So do you see a similarity between this story and the following one? Please comment
http://giffenman-miscellania.blogspot.com/2011/08/uk-tourists-beware-cambridge-hospital.htmlThursday, 25 August 2011
UK TOURISTS BEWARE – Cambridge Hospital Staff Demand Instant Money from Sick and Ailing Indian Tourist
Cambridge Hospital Staff Demand Instant Money from Sick and Ailing Indian Tourist
The UK likes to portray itself as a friendly and inviting place for tourists. Its visa regime informs tourists who possess medical insurance that in case of an emergency they will receive adequate medical treatment without any need to pay the money upfront. But this is not true in reality as the following story illustrates.
VM, aged 73, is an Indian tourist visiting her family in Cambridge UK since June 2011. On Thursday 18 Aug she was admitted to Cambridge's famous Addenbrooke's hospital for an emergency illness and she received good medical care. Her medical insurers contacted the hospital on Friday 19 August in order to confirm her medical insurance cover and to guarantee payment. Yet on Tuesday 23 August and Wednesday 24 August VM received a rude shock in her hospital bed. Staff from the finance department beseiged her sick bed and demanded that she sign a carte blanche document agreeing to pay any/all charges the NHS may levy for her treatment. When it was pointed out that her insurance company was willing to offer a payment guarantee for her treatment they refused to listen and threatened to deport the tourist.
This issue becomes even more important as London prepares to invite tourists for the 2012 Olympic games. As the following article shows, NHS hospitals have made it a policy to use such high handed behaviour to extort cash from patients in their ailing beds.
http://www.dailymail.co.uk/news/article-562980/Foreigners-asked-produce-cash-hospital-beds-crackdown-health-tourists.html
In short if this behaviour is allowed to continue, if a luckless tourist finds himself in an NHS hospital s/he will not only have to hope to get better soon in a foreign land, but also try to figure out how to arrange large amounts of cash to fob of the finance staff of these hospitals.
You have been warned, visit the UK only if you or your relatives have large amounts of instant cash. Else you and your relatives will be in peril should you have a medical emergency as NHS hospitals fail to honour the legal commitment made when you obtained your visa.
THE DAILY MAIL ARTICLE
Foreigners asked to produce cash in their hospital beds in crackdown on 'health tourists'
By OLINKA KOSTERLast updated at 17:54 30 April 2008
A hospital is pioneering a "get tough" attitude on health tourists - by throwing them out of hospital before their treatment is complete unless they pay up.
It means that foreigners who travel to Britain to get free care on the NHS will now be asked to produce cash or a credit card at their hospital bed.
The new approach has already saved the West Middlesex University Hospital in Isleworth up to £700,000 a year. Its proximity to Heathrow Airport makes it a particular target for immigrants.
If all hospitals did the same, the NHS could recoup tens of millions of pounds a year from health tourists.
Scroll down for more...
 Crackdown: West Middlessex University Hospital is getting tough on illegal 'health tourists'
Crackdown: West Middlessex University Hospital is getting tough on illegal 'health tourists'"We will discharge a patient before they are well," he insisted.
"We will discharge a patient when they are stable, when we have provided what we have to provide - the minimum benchmark.
"Generally, within the first 48 hours after admission they will be given a price on how much, roughly, their treatment is going to cost.
"If I'm interviewing an inpatient I will be at that patient's bedside and I will ask them there and then for a visa, MasterCard, debit card, or cash. We don't take cheques."
Under the current system, anyone who needs emergency care, such as for a heart attack or accident and emergency treatment after an accident, does not have to pay.
But patients not eligible for free care who attempt to use the NHS for ongoing care or treatment that is not immediately necessary have to pay.
These so-called health tourists normally receive a bill on departure from hospital - but only an estimated 30 per cent of the money is recovered.
Under the pilot scheme, they will be asked to pay at their hospital bed for non-emergency care, or told to leave.
However, they would only be discharged after three consultants have agreed their condition is stable.
In the case of a heart attack victim, NHS patients would normally stay in hospital for 10 days. But anyone not eligible for free care could be asked to leave after 48 hours if they are judged stable.
Most patients told to leave did so willingly, Mr Finlay added - but not all of them.
"I've had two death threats, I've been held up against a wall, I've been grabbed round the throat, I've been manhandled by relatives - verbal abuse is almost day-to-day," he said.
"You have to have a very thick skin."
Last year, a secret Government report based on figures from 12 NHS trusts suggested that the bill for treating health tourists was at least £62million a year.
This did not include the cost of treating foreigners entitled to free healthcare, such as asylum seekers and students.
Health tourists not entitled to free treatment include pregnant women who arrive on holiday visas and give birth here.
Many foreign HIV sufferers also target UK hospitals for treatment, the study from 2005 revealed.
In the case of an HIV patient, a clinical decision would be made as to whether emergency care was needed.
At the time the figures were revealed, Conservative MP Ben Wallace said hospitals appeared to be pursuing a "don't ask, don't charge and don't chase policy".
Cash-strapped hospitals are being pushed further into debt because they are failing to claim the millions owed to them by those abusing the system.
As well as the West Middlesex University Hospital, the Leeds Teaching Hospitals NHS Trust and the Luton and Dunstable NHS Foundation Trust have been chosen to take part in the pilot scheme because their catchment areas contain both a "major point of entry to the UK" and a large proportion of asylum seekers.
Mr Finlay said his methods had received an enthusiastic response from across Whitehall - and saved the trust between £600,000 and £700,000-a-year.
"They think it is a fantastic idea, a solution to a relatively new problem," he said.
"It is up to the Department of Health to see how brave they will be to use innovative ways to tackle health tourism."
A spokesman for the Department of Health said: "It is important that those who are not entitled to NHS services pay for any they receive.
"The Government is currently reviewing access to primary and secondary care for all foreign nationals.
"In doing this we must take into account the implications of any such decisions on the key preventative and public health responsibilities of the NHS.
"We always treat people and do not charge them for emergency treatment, but the thinking behind the pilot schemes is that the NHS is there first and foremost for people who live here."
Subscribe to:
Comments (Atom)

