Aakash Chopra in Cricinfo
The IPL is now nine seasons old. Having spent a few seasons in an IPL dressing room, I was soon convinced that T20 was here to stay, and second - a not-so-healthy upshot - that the format would seriously affect the growth of Test openers and spinners in particular. This because no other players are forced to change their basic game to suit the demands of the shortest format as much as Test openers and spinners.
A Test opener is a skeptic by nature. He is trained to distrust the ball till it reaches him. Early signs can be misleading; the ball might appear to be traveling in a straight line after the bowler releases it, but it's wrong for the batsman to assume that it will follow the same path till it reaches him. The new ball could move very late in the air or off the pitch, and so openers are hardwired to view it with suspicion. They are also trained not to commit early to a shot because that can leave them in a tangle. They're told to wait till the ball gets to them and play close to the body. Reaching out with the hands is a temptation a Test opener must guard against.
But in T20 cricket, an opener's role is to set the tone. Go really hard in the first six overs, which is when scoring is considered to be easiest. If you can't find the gaps, go aerial. If you can't go down straight, trust the bounce and go across. Don't get too close to the ball, as that will block the bat-swing. Stay away from the ball and use the arms and hands to reach out and hit. A spell of 12 balls without a boundary in the first six overs is considered to be pushing the team back. Patience might be a virtue in Tests; it's a liability in T20.
The same is true for the spinners. Flight, dip, guile and deception aren't the most sought after virtues in the world of T20. Instead, the focus is on keeping the trajectory low and bowling it a little quicker to discourage the batsmen from using their feet. Bounce is revered in Tests, but the lack of it is a boon in T20. We have seen spinners go extremely roundarm (remember Ravindra Jadeja in the IPL?) to prevent the batsman from getting under the bounce.
It takes a long time to master the art of bowling long spells to plot and plan dismissals in Test cricket - a tactic that's alien to T20 bowlers who are used to bowling four overs across two or more spells. You can't practise crossing the English Channel by spending 30 minutes in the swimming pool everyday. T20 cricket has challenged the fundamentals of spin bowling.
The reason I think middle-order batsmen and fast bowlers haven't been forced to change their game is because T20 hasn't demanded they do anything that they weren't already doing. A middle-order batsman in a Test side, as in a T20 game, is allowed to rotate the strike and play along the ground before accelerating the scoring. He does the same in Tests and ODIs, albeit later in the innings. The only adjustment he is called on to make is to shift gears a little sooner. That's easier to do than being asked to move from riding a bicycle to driving a sports car, as spinners and opening batsmen are.
Similarly, fast bowlers aren't pressed to do anything radically different either. Make the new ball swing, change lengths and pace regularly, and find the blockhole on demand. It's challenging for sure but not a skill-altering demand.
After weighing in these factors, it is only fair to assume that the next generation of spinners and openers for the longer format might take a lot longer to come to the fore, or worse, not do so at all. After all, why would somebody invest in the skill set required to play the longest format given the huge rewards on offer in the shortest format? Unless you just can't cut it in T20, leaving you with no choice whatsoever.
While the likes of David Warner and R Ashwin excel equally in both formats, it's worth noting that both honed their skills as youngsters when playing the longer format was still the way up. Also, both are aberrations and not the norm. Increasingly, Test teams are forced to pick specialists in these two departments.
KL Rahul comes across as the first to challenge my hypothesis, and perhaps he provides an insight into how cricketers of the future will be.
Things that look improbable now, both physically and mentally, could become reality in the near future. And Rahul's early success across formats offers proof. He was only 16 when the IPL started, in 2008, and his first-class debut came two years later, which makes him a wonderful case study.
Rahul is happy leaving the ball that is only a few inches outside the off stump in Tests, and equally adept at flaying anything wide. He puts in a long stride to get close to the ball and then lean into drives in the longer format, but in T20 he doesn't mind staying away from a ball pitched on the same length, the better to allow his hands to go through. Like a true Test opener, he is skeptical at the beginning of a Test innings, but he doesn't mind going down on one knee to scoop the first ball he faces in the shortest format.
He got out pulling from outside off in his debut Test match and since then he hasn't played that stroke early in his innings. By his own admission, he really enjoys playing the pull and hook to anything that is short. To shelve a shot that's dear to you in one format and play it in other formats shows discipline and patience. That's a virtue the new-age opener wasn't mastering, or so I thought.
Most importantly, a fifty or an eighty isn't enough for Rahul. In fact, save for one occasion, he has scored a century every time he has passed 50 in Tests. He has shown that if you train the mind as much as you train the body, it's indeed possible to find a game that's suited to Test cricket without compromising on success in other formats.
Over on the bowling side, we are still struggling to find spinners for the longer format. I won't be surprised if some boards decide to keep young spinners away from T20 cricket till a certain age, for it is widely accepted that the shortest format is affecting the development of young spinners.
Perhaps I'm taking Rahul's initial success too seriously. After all, he could be just like Warner, an aberration. But his style of play is reassuring and has given me hope. Maybe he's the first of the new breed of Test openers. Amen to that thought.
Simon Jenkins in The Guardian

‘I was touched, like everyone, by the Jason Kenny/Laura Trott ‘golden love bond’, but how many times did I need to see them in tears?’ Photograph: David Davies/PA
Australia’s cycling star, Anna Meares, said of Britain’s triumphant cyclists: “They’ve got it together … but, to be honest, I’m not exactly sure what they’ve got together.” The French and Germans were heard to murmur likewise. One interpretation could be that murky word “cheating”, although Meares strongly denied that she had ever suggested this. Given the recent history of the Olympics and the fierce pressure on British athletes, the accusation is pardonable. I doubt if it is true. What Britain “got together” was the money. Is that cheating?
I have intermittently enjoyed the Olympics on television. Mostly it is hours of flatulent BBC staff killing time by interviewing one another, interspersed with a few seconds of mostly baffling hysterics. Clare Balding appears in perpetual shriek: “Oh my God, I think our great British paint is drying faster than the Russian and the Colombian paint – but we must await a decision from the judges.”
Then on Tuesday night the BBC went bananas. At 10 o’clock we were denied important news – of Anjem Choudary’s conviction, of swingeing tax fines and of possible “special status” for Britain outside the EU. Instead we had to sit for an hour and a half, waiting for three minutes of BBC pandemonium as British cyclists yet again pedalled fast. We had to watch while the BBC aired pictures of its own commentary box punching the air and howling. These were not so much journalists as state cheerleaders. I was touched, like everyone, by the Jason Kenny/Laura Trott “golden love bond”, but how many times did I need to see them in tears? It was a total collapse of news values, the corporation peddling tabloid chauvinist schlock.
Throughout the cold war, Soviet bloc nations used sport as a proxy for economic success. With the connivance of the International Olympic Committee, they turned what used to be an amateur sport into the equivalent of a national defence force, hurling money and status at their athletes while the IOC turned the Games into a lavish field of the cloth of gold – at some poor taxpayer’s expense.
The west used to ridicule the communists for this. Their athletes were derided as state employees, civil servants and cheats. Of course many took drugs. Winning was what mattered to the Soviets, the state media being monopolised to convince their people that their “system” was better.
Since Atlanta in 1996, Britain has followed suit. The poor performance of British athletes was considered by John Major as a comment on his government. He demanded medals, and lots of them. The subsidy to “elite” sport was increased tenfold, from £5m to £54m, while popular sports facilities were closing. Money was directed specifically at disciplines where individuals could win multiple medals rather than just one, away from field athletics to cycling and gymnastics. It worked. The medals tally at Sydney 2000 rose from 15 to 28.
A UK Sport graph tracks the precise link between government grant (dressed up as lottery money) and Olympic medals. By 2012, this had risen to £264m, delivering 65 medals (just over £4m a medal). For Rio it has been £350m for the Olympics and Paralympics, with the target that Britain become “the first host nation to eclipse our London 2012 medal haul”.

Team GB's Olympics success shows UK can thrive outside EU, say Brexiters
No surprise, it is working. The best coaches were hired. Talent was ruthlessly selected and nurtured. Money was lavished on research, equipment, clothing and peak performance timing. The French and Germans noted that the British are doing far better in Rio than at recent world championships. Here clearly is one field in which British state investment knows how to pick winners.
Iain Dyer, Britain’s star cycling coach, talks like a Formula One boss. “We peaked in our research and innovation. The helmets were the 2012 ones, but the bikes are new, and different components and strategies are used for the first time.” Aerodynamic suits with magic chevrons are everywhere.
Rod Carr of UK Sport is equally open. He relates how the mix of penalties and incentives since Sydney led, in the case of gymnastics and swimming, to each sport thinking afresh and coming back with an investable proposition.
Athletes are unique among public servants in enjoying a hypothecated tax to give themselves up to £28,000 a year “to concentrate on training”. Poor countries can eat their hearts out.
I am thrilled by personal success, by Mo Farah’s 10,000m, Charlotte Dujardin’s horsemanship, Wayde van Niekerk’s 400m and Simone Biles’ mesmerising gymnastics. They are a joy to watch. But I do not mind their nationality. The nationalisation of sport – the hamfisted draping in the union jack after breasting the tape – so clearly diminishes the individual achievement. Ever since its introduction by Hitler at the 1936 Olympics, such chauvinism has infused democratic as well as authoritarian regimes. Olympic Games are like wars, foreign adventures offering regimes a salve to domestic woes. Athletes are recruited to the flag like soldiers. They are declared “heroes” and showered with honours.
For years, the Olympics were corrupted by shamateurism and drugs. The IOC, with British representatives present, knew perfectly well what was happening, but turned a blind eye. The most honest gold medal of recent years should have gone to the British media, alone in relentlessly revealing corruption and cheating in international sport. Yet it was accused by Britain’s Lord Coe of “a declaration of war on my sport”. When this was seen to be rubbish, he did not resign. He was declared an expert on sports ethics and appointed to the IOC. The Russians who blew the whistle on athletics doping are now forced to hide for their lives somewhere in America. These are the realities that should sit alongside the “heroism” of today’s games.
None of this explains the BBC, which has brought Rio close to a British National party awayday. The Chinese had it right. They used to dedicate their medals to the Chinese Communist party and people, who after all had paid for them. As for the accusations against Britain’s cyclists, the response is simple. Who needs to cheat with drugs when medals go to money? Perhaps the best answer is for countries that have no money to be allowed drugs, to level the playing field. They are cheaper.
Ranjana Srivastava in The Guardian
Our consultation is nearly finished when my patient leans forward, and says, “So, doctor, in all this time, no one has explained this. Exactly how will I die?” He is in his 80s, with a head of snowy hair and a face lined with experience. He has declined a second round of chemotherapy and elected to have palliative care. Still, an academic at heart, he is curious about the human body and likes good explanations.
“What have you heard?” I ask. “Oh, the usual scary stories,” he responds lightly; but the anxiety on his face is unmistakable and I feel suddenly protective of him.
“Would you like to discuss this today?” I ask gently, wondering if he might want his wife there.
“As you can see I’m dying to know,” he says, pleased at his own joke.
If you are a cancer patient, or care for someone with the illness, this is something you might have thought about. “How do people die from cancer?” is one of the most common questions asked of Google. Yet, it’s surprisingly rare for patients to ask it of their oncologist. As someone who has lost many patients and taken part in numerous conversations about death and dying, I will do my best to explain this, but first a little context might help.
Some people are clearly afraid of what might be revealed if they ask the question. Others want to know but are dissuaded by their loved ones. “When you mention dying, you stop fighting,” one woman admonished her husband. The case of a young patient is seared in my mind. Days before her death, she pleaded with me to tell the truth because she was slowly becoming confused and her religious family had kept her in the dark. “I’m afraid you’re dying,” I began, as I held her hand. But just then, her husband marched in and having heard the exchange, was furious that I’d extinguish her hope at a critical time. As she apologised with her eyes, he shouted at me and sent me out of the room, then forcibly took her home.
It’s no wonder that there is reluctance on the part of patients and doctors to discuss prognosis but there is evidence that truthful, sensitive communication and where needed, a discussion about mortality, enables patients to take charge of their healthcare decisions, plan their affairs and steer away from unnecessarily aggressive therapies. Contrary to popular fears, patients attest that awareness of dying does not lead to greater sadness, anxiety or depression. It also does not hasten death. There is evidence that in the aftermath of death, bereaved family members report less anxiety and depression if they were included in conversations about dying. By and large, honesty does seem the best policy.
Studies worryingly show that a majority of patients are unaware of a terminal prognosis, either because they have not been told or because they have misunderstood the information. Somewhat disappointingly, oncologists who communicate honestly about a poor prognosis may be less well liked by their patient. But when we gloss over prognosis, it’s understandably even more difficult to tread close to the issue of just how one might die.
Thanks to advances in medicine, many cancer patients don’t die and the figures keep improving. Two thirds of patients diagnosed with cancer in the rich world today will survive five years and those who reach the five-year mark will improve their odds for the next five, and so on. But cancer is really many different diseases that behave in very different ways. Some cancers, such as colon cancer, when detected early, are curable. Early breast cancer is highly curable but can recur decades later. Metastatic prostate cancer, kidney cancer and melanoma, which until recently had dismal treatment options, are now being tackled with increasingly promising therapies that are yielding unprecedented survival times.
But the sobering truth is that advanced cancer is incurable and although modern treatments can control symptoms and prolong survival, they cannot prolong life indefinitely. This is why I think it’s important for anyone who wants to know, how cancer patients actually die.
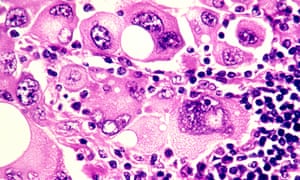
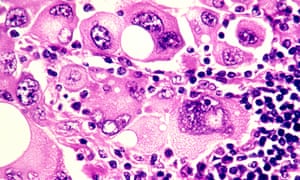
‘Cancer cells release a plethora of chemicals that inhibit appetite and affect the digestion and absorption of food’ Photograph: Phanie / Alamy/Alamy
“Failure to thrive” is a broad term for a number of developments in end-stage cancer that basically lead to someone slowing down in a stepwise deterioration until death. Cancer is caused by an uninhibited growth of previously normal cells that expertly evade the body’s usual defences to spread, or metastasise, to other parts. When cancer affects a vital organ, its function is impaired and the impairment can result in death. The liver and kidneys eliminate toxins and maintain normal physiology – they’re normally organs of great reserve so when they fail, death is imminent.
Cancer cells release a plethora of chemicals that inhibit appetite and affect the digestion and absorption of food, leading to progressive weight loss and hence, profound weakness. Dehydration is not uncommon, due to distaste for fluids or an inability to swallow. The lack of nutrition, hydration and activity causes rapid loss of muscle mass and weakness. Metastases to the lung are common and can cause distressing shortness of breath – it’s important to understand that the lungs (or other organs) don’t stop working altogether, but performing under great stress exhausts them. It’s like constantly pushing uphill against a heavy weight.
Cancer patients can also die from uncontrolled infection that overwhelms the body’s usual resources. Having cancer impairs immunity and recent chemotherapy compounds the problem by suppressing the bone marrow. The bone marrow can be considered the factory where blood cells are produced – its function may be impaired by chemotherapy or infiltration by cancer cells.Death can occur due to a severe infection. Pre-existing liver impairment or kidney failure due to dehydration can make antibiotic choice difficult, too.
You may notice that patients with cancer involving their brain look particularly unwell. Most cancers in the brain come from elsewhere, such as the breast, lung and kidney. Brain metastases exert their influence in a few ways – by causing seizures, paralysis, bleeding or behavioural disturbance. Patients affected by brain metastases can become fatigued and uninterested and rapidly grow frail. Swelling in the brain can lead to progressive loss of consciousness and death.
In some cancers, such as that of the prostate, breast and lung, bone metastases or biochemical changes can give rise to dangerously high levels of calcium, which causes reduced consciousness and renal failure, leading to death.
Uncontrolled bleeding, cardiac arrest or respiratory failure due to a large blood clot happen – but contrary to popular belief, sudden and catastrophic death in cancer is rare. And of course, even patients with advanced cancer can succumb to a heart attack or stroke, common non-cancer causes of mortality in the general community.
You may have heard of the so-called “double effect” of giving strong medications such as morphine for cancer pain, fearing that the escalation of the drug levels hastens death. But experts say that opioids are vital to relieving suffering and that they typically don’t shorten an already limited life.
It’s important to appreciate that death can happen in a few ways, so I wanted to touch on the important topic of what healthcare professionals can do to ease the process of dying.
In places where good palliative care is embedded, its value cannot be overestimated. Palliative care teams provide expert assistance with the management of physical symptoms and psychological distress. They can address thorny questions, counsel anxious family members, and help patients record a legacy, in written or digital form. They normalise grief and help bring perspective at a challenging time.
People who are new to palliative care are commonly apprehensive that they will miss out on effective cancer management but there is very good evidence that palliative care improves psychological wellbeing, quality of life, and in some cases, life expectancy. Palliative care is a relative newcomer to medicine, so you may find yourself living in an area where a formal service doesn’t exist, but there may be local doctors and allied health workers trained in aspects of providing it, so do be sure to ask around.
Finally, a word about how to ask your oncologist about prognosis and in turn, how you will die. What you should know is that in many places, training in this delicate area of communication is woefully inadequate and your doctor may feel uncomfortable discussing the subject. But this should not prevent any doctor from trying – or at least referring you to someone who can help.
Accurate prognostication is difficult, but you should expect an estimation in terms of weeks, months, or years. When it comes to asking the most difficult questions, don’t expect the oncologist to read between the lines. It’s your life and your death: you are entitled to an honest opinion, ongoing conversation and compassionate care which, by the way, can come from any number of people including nurses, social workers, family doctors, chaplains and, of course, those who are close to you.
Over 2,000 years ago, the Greek philosopher Epicurus observed that the art of living well and the art of dying well were one. More recently, Oliver Sacks reminded us of this tenet as he was dying from metastatic melanoma. If die we must, it’s worth reminding ourselves of the part we can play in ensuring a death that is peaceful.
Polly Toynbee in The Guardian
A fish rots from the head, but the NHS may be rotting from the feet. Podiatry is not up there in the headlines, yet what’s going on in that unglamorous zone is an alarming microcosm of the downward path of the health service. This is a story of the NHS in England in retreat and the private sector filling the vacuum.
You know the big picture from the ever-worsening monthly figures: deteriorating A&E, ambulance and operation waiting times, and a steep rise in bed-blocking. As debts pass £2.5bn, the NHS feels the tightening financial tourniquet.
Now look at it through the prism of just one small corner, as seen from the feet up. Every week 135 people have amputations because diabetes has caused their feet to rot: their circulation goes and then the sensation in their feet, so they don’t notice damage done by rubbing shoes, stubbed toes or stepping on nails. Minor injuries turn into ulcers that if left untreated turn gangrenous, and so the toes, then the foot, then the leg are lost – horrific life-changing damage. Numbers are rising fast, with nearly three million diabetics. The scandal is that 80% of these amputations are preventable – if there were the podiatrists to treat the first signs of foot ulcers. But the numbers employed and in training are falling.
In his surgery, the head of podiatry for Solent NHS Trust, Graham Bowen, is unwrapping the foot of a lifelong diabetic to reveal a large missing chunk of heel, a great red hole nearly through to the bone. This man has already had some toes amputated. He has been having treatment with maggots, bandaged into his wound to eat the dead skin and help healing – and he is slowly improving. Everyone Bowen sees now is at similarly high risk. Small ulcers, incipient ulcers, the ones that need to be caught early (and cheaply) no longer get NHS treatment. “On the NHS we’re essentially firefighting the worst cases now,” says Bowen. “We are going through our lists and discharging all the rest of our patients.”

FacebookTwitterPinterest ‘On a 15-minute visit carers can’t check feet.’ Photograph: Andrew Bret Wallis/Getty Images
But not even all these acute patients get the same optimal treatments, due to the vagaries of the 2012 NHS Act. Solent, a community trust that covers mental health and a host of other services, is used by five different clinical commissioning groups (CCGs), including Southampton, Portsmouth and West Hampshire. Each has its own criteria for what it will pay for, and each is toughening those criteria. Depending on their address, some patients get the very best, others only get what their cash-strapped CCG pays for.
You need to know about diabetic feet to understand the difference in treatments: the conventional and cheapest treatment is a dressing and a removable plastic boot, and telling patients to keep their foot up for months. But patients who can’t feel their feet tend to take off the boot and hobble to make a quick cup of tea. “Ten minutes of putting pressure on the ulcer undoes 23 hours of resting it,” Bowen says, so it takes 52 weeks on average to heal ulcers that way. For £500 extra, a new instant fibreglass cast saves any pressure on ulcers and cures them within eight weeks.
Although the National Institute for Health and Care Excellence says this total-contact cast is the gold standard, most of Bowen’s CCGs won’t pay for it. I watched him putting one on a patient in under half an hour: after nine weekly replacements, that ulcer would be completely healed. For every 10 of the new casts, one amputation is prevented – and each amputation costs the NHS £65,000. Such is the madness of NHS fragmentation, divided between multiple commissioners and providers, all in serious financial trouble, that no one spends a bit more now for others to save later, even when the payback is so quick.
This clinic lost four podiatry posts to save money: though diabetic numbers soar, its budget has been static for five years. “Doing more for less,” he says with the same weary sigh you hear echoing through the NHS. As Bowen goes through the clinic’s books removing all but the most acute cases, he turns away diabetics whose problems should be caught early. He turns away others he used to treat: the old and frail who have become immobile due to foot problems; the partially sighted or people with dementia who have poor home care. On a 15-minute visit carers can’t check feet and find out if they are the reason someone doesn’t get out of bed, toes buckled in, leaving them needlessly incapacitated and heading for residential care sooner than necessary.
What happens to those he takes off his books? “They have to go private, if they can afford it. If not, then nothing.” He used to send them to Age UK, but lack of funds shut that service. Only 5% of podiatry is now done by the NHS so Bowen has set up TipToe, a private practice attached to his NHS clinic. It’s not what he wants, but it keeps prices low and all proceeds go to the NHS.
Alarm bells should ring here: how silently the NHS slides into the private sector. Labour leadership contender Owen Smith has flagged up his team’s research showing private practice has doubled since 2010. Now that many CCGs only pay for one cataract, how many go private for the second eye? As the Guardian’s health policy editor, Denis Campbell, has asked, how many more vital treatments will go this way?
Podiatry is the ground floor of the NHS hierarchy. The profession reckons the NHS in England needs 12,000 practitioners but only has about 3,000 – and that’s falling, despite so many high-risk diabetics needing weekly appointments. Next year podiatry trainees, like nurses, will no longer receive state bursaries, so fewer will apply. They tend to be older, with families, unable to take on a £45,000 debt for a job paying around £35,000 per year. Already student places have been cut by nearly a quarter in five years. Most of the 7,000 amputations a year are preventable. A shocking statistic: half of those who undergo amputations will die within two years.
Only in the details of what’s happening on the frontline can we understand the daily reality of Britain’s shrinking state. Step back and ask how it can be that a country still growing richer can afford less quality care than when it was poorer? Is that the country’s choice? As the NHS slides into the private sector, here is yet another public service in retreat.