'People will forgive you for being wrong, but they will never forgive you for being right - especially if events prove you right while proving them wrong.' Thomas Sowell
Search This Blog
Showing posts with label opium. Show all posts
Showing posts with label opium. Show all posts
Sunday, 5 June 2022
Thursday, 8 November 2018
The making of an opioid epidemic
When high doses of painkillers led to widespread addiction, it was called one of the biggest mistakes in modern medicine. But this was no accident. By Chris McGreal in The Guardian
Jane Ballantyne was, at one time, a true believer. The British-born doctor, who trained as an anaesthetist on the NHS before her appointment to head the pain department at Harvard and its associated hospital, drank up the promise of opioid painkillers – drugs such as morphine and methadone – in the late 1990s. Ballantyne listened to the evangelists among her colleagues who painted the drugs as magic bullets against the scourge of chronic pain blighting millions of American lives. Doctors such as Russell Portenoy at the Memorial Sloan Kettering Cancer Center in New York saw how effective morphine was in easing the pain of dying cancer patients thanks to the hospice movement that came out of the UK in the 1970s.
Why, the new thinking went, could the same opioids not be made to work for people grappling with the physical and mental toll of debilitating pain from arthritis, wrecked knees and bodies worn out by physically demanding jobs? As Portenoy saw it, opiates were effective painkillers through most of recorded history and it was only outdated fears about addiction that prevented the drugs still playing that role.
Opioids were languishing from the legacy of an earlier epidemic that prompted President Theodore Roosevelt to appoint the US’s first opium commissioner, Dr Hamilton Wright, in 1908. Portenoy wanted to liberate them from this taint. Wright described Americans as “the greatest drug fiends in the world”, and opium and morphine as a “national curse”. After that the medical profession treated opioid pain relief with what Portenoy and his colleagues regarded as unwarranted fear, stigmatising a valuable medicine.
These new evangelists painted a picture of a nation awash in chronic pain that could be relieved if only the medical profession would overcome its prejudices. They constructed a web of claims they said were rooted in science to back their case, including an assertion that the risk of addiction from narcotic painkillers was “less than 1%” and that dosages could be increased without limit until the pain was overcome. But the evidence was, at best, thin and in time would not stand up to detailed scrutiny. One theory, promoted by Dr David Haddox, was that patients genuinely experiencing pain could not become addicted to opioids because the pain neutralised the euphoria caused by the narcotic. He said that what looked to prescribing doctors like a patient hooked on the drug was “pseudo-addiction”.
Portenoy toured the country, describing opioids as a gift from nature and promoting access to narcotics as a moral argument. Being pain-free was a human right, he said. In 1993, he told the New York Times of a “growing literature showing that these drugs can be used for a long time, with few side-effects, and that addiction and abuse are not a problem”.
Long after the epidemic took hold, and the death toll rose into the hundreds of thousands in the US, Portenoy admitted that there was little basis for this claim and that he had been more interested in changing attitudes to opioids among doctors than in scientific rigour.
“In essence, this was education to destigmatise and because the primary goal was to destigmatise, we often left evidence behind,” he admitted years later as the scale of the epidemic unfolded.
Likewise, Haddox’s theory of pseudo-addiction was based on the study of a single cancer patient. At the time, though, the new thinking was a liberation for primary care doctors frustrated at the limited help they could offer patients begging to get a few hours’ sleep. Ballantyne was as enthusiastic as anyone and began teaching the gospel of pain relief at Harvard, and embracing opioids to treat her patients.
“Our message was a message of hope,” she said. “We were teaching that we shouldn’t withhold opiates from people suffering from chronic pain and that the risks of addiction were pretty low because that was the teaching we’d received.”
But then Ballantyne began to see signs in her patients that experience wasn’t matching theory. Doctors were told they could repeatedly ratchet up the dosage of narcotics and switch to a new and powerful drug, OxyContin, without endangering the patient, because the pain, in effect, cancelled out the risk of addiction. To her dismay, Ballantyne saw that many of her patients were not better off when taking the drugs and were showing signs of dependence.
Among those patients on high doses over months and years, Ballantyne heard from one after another that the more drugs they took, the worse their pain became. But if they tried to stop or cut back on the pills, their pain also worsened. They were trapped.
“You had never seen people in such agony as these people on high doses of opiates,” she told me. “And we thought it’s not just because of the underlying pain; it’s to do with the medication.”
As Ballantyne listened to relatives of her patients talk about how much the drugs had changed their loved ones, her misgivings grew. Husbands spoke of wives as if a part of them were lost. Mothers complained that children had become sullen and distant, their judgment gone, their personality warped, their character altered. None of this should have been happening. Pain relief was supposed to free the patients, not imprison them. It was all very far from the promise of a magic bullet.
As the evidence that opioids were not delivering as promised piled up, the Harvard specialist began to record her findings. By then, though, there were other powerful forces with a big financial stake in the wider prescribing of painkilling drugs. Pharmaceutical companies are not slow to spot an opportunity and the push for wider prescribing of opioids had not gone unnoticed by the drug-makers, including the manufacturer of OxyContin, Purdue Pharma, which rapidly came to play a central role in the epidemic.
As the influence of the opioid evangelists grew, and restraints on prescribing loosened, the pharmaceutical industry moved to the fore with a push to make opioids the default treatment for pain, and to take advantage of the huge profits to be made from mass prescribing of a drug that was cheap to produce.
Jane Ballantyne was, at one time, a true believer. The British-born doctor, who trained as an anaesthetist on the NHS before her appointment to head the pain department at Harvard and its associated hospital, drank up the promise of opioid painkillers – drugs such as morphine and methadone – in the late 1990s. Ballantyne listened to the evangelists among her colleagues who painted the drugs as magic bullets against the scourge of chronic pain blighting millions of American lives. Doctors such as Russell Portenoy at the Memorial Sloan Kettering Cancer Center in New York saw how effective morphine was in easing the pain of dying cancer patients thanks to the hospice movement that came out of the UK in the 1970s.
Why, the new thinking went, could the same opioids not be made to work for people grappling with the physical and mental toll of debilitating pain from arthritis, wrecked knees and bodies worn out by physically demanding jobs? As Portenoy saw it, opiates were effective painkillers through most of recorded history and it was only outdated fears about addiction that prevented the drugs still playing that role.
Opioids were languishing from the legacy of an earlier epidemic that prompted President Theodore Roosevelt to appoint the US’s first opium commissioner, Dr Hamilton Wright, in 1908. Portenoy wanted to liberate them from this taint. Wright described Americans as “the greatest drug fiends in the world”, and opium and morphine as a “national curse”. After that the medical profession treated opioid pain relief with what Portenoy and his colleagues regarded as unwarranted fear, stigmatising a valuable medicine.
These new evangelists painted a picture of a nation awash in chronic pain that could be relieved if only the medical profession would overcome its prejudices. They constructed a web of claims they said were rooted in science to back their case, including an assertion that the risk of addiction from narcotic painkillers was “less than 1%” and that dosages could be increased without limit until the pain was overcome. But the evidence was, at best, thin and in time would not stand up to detailed scrutiny. One theory, promoted by Dr David Haddox, was that patients genuinely experiencing pain could not become addicted to opioids because the pain neutralised the euphoria caused by the narcotic. He said that what looked to prescribing doctors like a patient hooked on the drug was “pseudo-addiction”.
Portenoy toured the country, describing opioids as a gift from nature and promoting access to narcotics as a moral argument. Being pain-free was a human right, he said. In 1993, he told the New York Times of a “growing literature showing that these drugs can be used for a long time, with few side-effects, and that addiction and abuse are not a problem”.
Long after the epidemic took hold, and the death toll rose into the hundreds of thousands in the US, Portenoy admitted that there was little basis for this claim and that he had been more interested in changing attitudes to opioids among doctors than in scientific rigour.
“In essence, this was education to destigmatise and because the primary goal was to destigmatise, we often left evidence behind,” he admitted years later as the scale of the epidemic unfolded.
Likewise, Haddox’s theory of pseudo-addiction was based on the study of a single cancer patient. At the time, though, the new thinking was a liberation for primary care doctors frustrated at the limited help they could offer patients begging to get a few hours’ sleep. Ballantyne was as enthusiastic as anyone and began teaching the gospel of pain relief at Harvard, and embracing opioids to treat her patients.
“Our message was a message of hope,” she said. “We were teaching that we shouldn’t withhold opiates from people suffering from chronic pain and that the risks of addiction were pretty low because that was the teaching we’d received.”
But then Ballantyne began to see signs in her patients that experience wasn’t matching theory. Doctors were told they could repeatedly ratchet up the dosage of narcotics and switch to a new and powerful drug, OxyContin, without endangering the patient, because the pain, in effect, cancelled out the risk of addiction. To her dismay, Ballantyne saw that many of her patients were not better off when taking the drugs and were showing signs of dependence.
Among those patients on high doses over months and years, Ballantyne heard from one after another that the more drugs they took, the worse their pain became. But if they tried to stop or cut back on the pills, their pain also worsened. They were trapped.
“You had never seen people in such agony as these people on high doses of opiates,” she told me. “And we thought it’s not just because of the underlying pain; it’s to do with the medication.”
As Ballantyne listened to relatives of her patients talk about how much the drugs had changed their loved ones, her misgivings grew. Husbands spoke of wives as if a part of them were lost. Mothers complained that children had become sullen and distant, their judgment gone, their personality warped, their character altered. None of this should have been happening. Pain relief was supposed to free the patients, not imprison them. It was all very far from the promise of a magic bullet.
As the evidence that opioids were not delivering as promised piled up, the Harvard specialist began to record her findings. By then, though, there were other powerful forces with a big financial stake in the wider prescribing of painkilling drugs. Pharmaceutical companies are not slow to spot an opportunity and the push for wider prescribing of opioids had not gone unnoticed by the drug-makers, including the manufacturer of OxyContin, Purdue Pharma, which rapidly came to play a central role in the epidemic.
As the influence of the opioid evangelists grew, and restraints on prescribing loosened, the pharmaceutical industry moved to the fore with a push to make opioids the default treatment for pain, and to take advantage of the huge profits to be made from mass prescribing of a drug that was cheap to produce.
Bottles of painkiller OxyContin, made by Purdue Pharma. Photograph: Reuters
The American Pain Society, a body partially funded by pharmaceutical companies, was pushing the concept of pain as the “fifth vital sign”, alongside other measures of health such as heart rate and blood pressure. “Vital signs are taken seriously,” said its president, James Campbell, in a 1996 speech to the society. “If pain were assessed with the same zeal as other vital signs are, it would have a much better chance of being treated properly. We need to train doctors and nurses to treat pain as a vital sign.”
The APS wanted the practice of checking pain as a vital sign as a matter of routine adopted in American hospitals. The key was to win over the Joint Commission for Accreditation of Healthcare Organizations, which certifies about 20,000 hospitals and clinics in the US. Its stamp of approval is the gateway for medical facilities to tap into the huge pot of federal money paying for healthcare for older, disabled and poor people. Hospitals are careful not to get on the wrong side of the joint commission’s “best practices” or to fail its regular performance reviews.
In response to what it called “the national outcry about the widespread problem of under-treatment” – an outcry in good part generated by drug manufacturers – the commission issued new standards for pain care in 2001. Hospital administrators picked over the document to ensure they understood exactly what was required.
Every patient was to be asked about their pain levels, no matter what the reason they were seeing a doctor. Hospitals adopted a system of colour-coded smiley faces, to represent a rising scale of pain from 0-10. The commission ruled that anybody identifying as a five – a yellow neutral face described as “very distressing” – or above was to be was to be referred for a pain consultation.
The commission told hospitals they would be expected to meet the new standards for pain management at their next accreditation survey. Purdue Pharma was ready. The company offered to distribute materials to educate doctors in pain management for free. This amounted to exclusive rights to indoctrinate medical staff. A training video asserted that there is “no evidence that addiction is a significant issue when persons are given opioids for pain control”, and claimed that some clinicians had “inaccurate and exaggerated concerns about addiction, tolerance and risk of death”. Neither claim was true.
Some doctors questioned the value of patient self-assessment, but the commission’s regulations soon came to be viewed as a rigid standard. In time, pain as the fifth vital sign worked its way into hospital culture. New generations of nurses, steeped in the opioid orthodoxy, sometimes came to see pain as more important than other health indicators.
Dr Roger Chou, a pain specialist at Oregon Health and Science University who has made long-term studies of the effectiveness of opioid painkillers and helped shape the Centers for Disease Control and Prevention’s policy on the epidemic, said the focus on pain caused patients to give it greater weight than made sense.
“When you start asking people: ‘How much pain are you having?’ every time they come into the hospital, then people start thinking: ‘Well, maybe I shouldn’t be having this little ache I’ve been having. Maybe there’s something wrong.’ You’re medicalising what’s a normal part of life,” he said.
One consequence was that people with relatively minor pain were increasingly directed toward medicinal treatment while consideration of safer or more effective alternatives, such as physiotherapy, were marginalised. Another, said Chou, was the increased expectation that pain can be eliminated. Chasing the lowest score on the pain chart often came at the expense of quality of life as opioid doses increased. “It’s better to have a little bit of pain and be functional than to have no pain and be completely unfunctional,” said Chou.
Health insurance companies piled yet more pressure on doctors to follow the path of least resistance. This meant cutting consultation times and payments for more costly forms of pain treatment in favour of the direct approach: drugs.
The joint commission needed a way to judge whether its 2001 edict on pain was being adhered to and latched on to patient satisfaction surveys. It took a determined doctor to resist the pressure to prescribe. Physicians could spend half an hour pressing a person to take more responsibility for their own health – eat better, exercise more, drink less, find ways to deal with stress – only to watch an unhappy patient make their views known on the satisfaction survey and face a dressing down from hospital management. Or they could quickly do what the patient came in for: give them a pill and get full marks.
In Detroit, Dr Charles Lucas’s three decades of experience as a surgeon told him it was possible to what was easy and sign the prescription, or to do what was hard. Lucas grew up in the city and had been instrumental in establishing Detroit’s publicly owned hospital as the highest-level trauma centre in Michigan and one of the first top-tier centres in the country.
The American Pain Society, a body partially funded by pharmaceutical companies, was pushing the concept of pain as the “fifth vital sign”, alongside other measures of health such as heart rate and blood pressure. “Vital signs are taken seriously,” said its president, James Campbell, in a 1996 speech to the society. “If pain were assessed with the same zeal as other vital signs are, it would have a much better chance of being treated properly. We need to train doctors and nurses to treat pain as a vital sign.”
The APS wanted the practice of checking pain as a vital sign as a matter of routine adopted in American hospitals. The key was to win over the Joint Commission for Accreditation of Healthcare Organizations, which certifies about 20,000 hospitals and clinics in the US. Its stamp of approval is the gateway for medical facilities to tap into the huge pot of federal money paying for healthcare for older, disabled and poor people. Hospitals are careful not to get on the wrong side of the joint commission’s “best practices” or to fail its regular performance reviews.
In response to what it called “the national outcry about the widespread problem of under-treatment” – an outcry in good part generated by drug manufacturers – the commission issued new standards for pain care in 2001. Hospital administrators picked over the document to ensure they understood exactly what was required.
Every patient was to be asked about their pain levels, no matter what the reason they were seeing a doctor. Hospitals adopted a system of colour-coded smiley faces, to represent a rising scale of pain from 0-10. The commission ruled that anybody identifying as a five – a yellow neutral face described as “very distressing” – or above was to be was to be referred for a pain consultation.
The commission told hospitals they would be expected to meet the new standards for pain management at their next accreditation survey. Purdue Pharma was ready. The company offered to distribute materials to educate doctors in pain management for free. This amounted to exclusive rights to indoctrinate medical staff. A training video asserted that there is “no evidence that addiction is a significant issue when persons are given opioids for pain control”, and claimed that some clinicians had “inaccurate and exaggerated concerns about addiction, tolerance and risk of death”. Neither claim was true.
Some doctors questioned the value of patient self-assessment, but the commission’s regulations soon came to be viewed as a rigid standard. In time, pain as the fifth vital sign worked its way into hospital culture. New generations of nurses, steeped in the opioid orthodoxy, sometimes came to see pain as more important than other health indicators.
Dr Roger Chou, a pain specialist at Oregon Health and Science University who has made long-term studies of the effectiveness of opioid painkillers and helped shape the Centers for Disease Control and Prevention’s policy on the epidemic, said the focus on pain caused patients to give it greater weight than made sense.
“When you start asking people: ‘How much pain are you having?’ every time they come into the hospital, then people start thinking: ‘Well, maybe I shouldn’t be having this little ache I’ve been having. Maybe there’s something wrong.’ You’re medicalising what’s a normal part of life,” he said.
One consequence was that people with relatively minor pain were increasingly directed toward medicinal treatment while consideration of safer or more effective alternatives, such as physiotherapy, were marginalised. Another, said Chou, was the increased expectation that pain can be eliminated. Chasing the lowest score on the pain chart often came at the expense of quality of life as opioid doses increased. “It’s better to have a little bit of pain and be functional than to have no pain and be completely unfunctional,” said Chou.
Health insurance companies piled yet more pressure on doctors to follow the path of least resistance. This meant cutting consultation times and payments for more costly forms of pain treatment in favour of the direct approach: drugs.
The joint commission needed a way to judge whether its 2001 edict on pain was being adhered to and latched on to patient satisfaction surveys. It took a determined doctor to resist the pressure to prescribe. Physicians could spend half an hour pressing a person to take more responsibility for their own health – eat better, exercise more, drink less, find ways to deal with stress – only to watch an unhappy patient make their views known on the satisfaction survey and face a dressing down from hospital management. Or they could quickly do what the patient came in for: give them a pill and get full marks.
In Detroit, Dr Charles Lucas’s three decades of experience as a surgeon told him it was possible to what was easy and sign the prescription, or to do what was hard. Lucas grew up in the city and had been instrumental in establishing Detroit’s publicly owned hospital as the highest-level trauma centre in Michigan and one of the first top-tier centres in the country.
Activists in New York, during a protest denouncing the city’s ‘inadequate and wrongheaded response’ to the opioid overdose crisis. Photograph: Getty
Emergency departments became beacons for the opioid dependent, who quickly learned to game the system to get drugs on top of their prescriptions. They turned up feigning pain, knowing harassed medical staff under pressure of time and the commission’s standards were likely to prescribe narcotics and move on without too many questions.
“Some of the old-time nurses, they have that jaundiced look in their eye and say ‘So-and-so’s complaining of pain’. You can tell by the look in their eye that they don’t think it’s justified that they get any more medicine,” said Lucas. “The younger nurses, they say we have to treat this pain – because they’ve been indoctrinated – they’ve got to get rid of the pain. God forbid you don’t get rid of the pain. That would be like a mortal sin.”
But there was a price for resisting the pressure to prescribe ever higher doses of pain relief.
Lucas was knocked back in surprise, and then infuriated, to be summoned to appear before his hospital’s ethics committee after a nurse reported him for failing to provide adequate pain treatment.
The surgeon’s longstanding patients included Gail Purton, the wife of a well-known Michigan radio personality. Lucas operated on Purton a few times, and she was back for surgery after her ovarian cancer spread. “It was a big operation. Cut off all sorts of cancer.” The next day, a nurse asked Purton if she was in pain. Purton said she was. The nurse reported Lucas for failing to properly address a patient’s pain. “I got reported because I wasn’t giving her enough pain medicine. She had a big cut from here to here,” Lucas said, running his finger across the front of his shirt and scoffing at the idea that she could be pain-free after an operation like that.
The surgeon responded with a five-page letter to the ethics committee chairman, whom he happened to have trained, challenging the questioning of his professional judgment. Purton wrote her own letter, praising Lucas’s care and saying that she never expected not to have pain after a major operation.
The case was dropped, but it was not an isolated incident. Lucas has worked closely with another surgeon, Anna Ledgerwood, since 1972. She too was hauled before the ethics committee on more than one occasion, on the same charge. It cleared Ledgerwood, but Lucas said more junior surgeons buckled to the pressure to administer opioids just to stay out of trouble.
Lucas regarded the new pain orthodoxy as a growing tyranny. He also thought it was killing patients. He began to collect his own data.
As the joint commission was pushing out its new standards for pain treatment in the early 2000s, the industry was driving a parallel effort to influence the prescribing habits of doctors in small clinics and private practices across the country. Many were still hesitant to prescribe narcotics, in part because of fear of legal liability for overdose or addiction.
The American Pain Society and Haddox, who was by then working for Purdue Pharma, were instrumental in writing a policy document reassuring doctors they would not face disciplinary action for prescribing narcotics, even in large quantities. The industry latched on to the Federation of State Medical Boards because of its influence over health policy individual US states which regulate how doctors practise medicine.
In 2001, Purdue Pharma funded the distribution of new pain treatment guidelines drawn up by the FSMB that sounded many of the same themes as the standards written by the joint commission.
The document picked up on Haddox’s pseudo-addiction theory. “Physicians should recognise that tolerance and physical dependence are normal consequences of sustained use of opioid analgesics and are not synonymous with addiction,” it said.
The FSMB pressed state medical boards to adopt the guidelines and to reassure doctors that adhering to them would diminish the likelihood of disciplinary action.
Over the following decade, the FSMB took close to $2m (£1.52m) from the drug industry, which mostly went to promote the guidelines and to finance a book, Responsible Opioid Prescribing, written with the oversight and advice of a clutch of doctors who were strong advocates of wider use of prescription narcotics. The book was sold to state medical boards and health departments for distribution to physicians, clinics and hospitals. The drug industry paid for the publication but the FSMB kept the $270,000 profits from sales.
Within a few years, the model guidelines were adopted in full or in part by 35 states, and the floodgates were open to mass prescribing of what Drug Enforcement Administration agents came to call “heroin in a pill”. Opioids were soon the default treatment even for relatively minor pain. Dentists gave them to teenagers after pulling their wisdom teeth. Not just one or two days’ worth of pills, but a fortnight or a month’s worth, which, if they did not draw the intended recipient in, frequently sat in the medicine cabinet waiting to be discovered by someone else in the family. The lack of caution in prescribing left an impression among the users that the drugs were harmless, and some people shared them with others as easily as they might an aspirin. Prescribing escalated year on year. So did profits. OxyContin sales passed $1bn a year in 2000. Three years later they were twice that. Other opioid makers were pulling in huge profits too.
By the time the FSMB guidelines were landing in doctors’ inboxes in the early 2000s, Ballantyne had reached her own conclusions about the impact of escalating opioid prescribing. In 2003, she co-authored an article in the New England Journal of Medicine highlighting the dearth of comprehensive trials and saying that two important questions remained unanswered even as mass prescribing of opioids took off. Do they work long term? Are higher doses safe to take year after year? The drug industry and opioid evangelists said yes, but where was the evidence for it?
Ballantyne wrote that there was evidence that putting some patients on serial prescriptions of strong opioids has the opposite of the intended effect. High doses not only build up a tolerance to the drug, but cause increased sensitivity to pain. The drugs were defeating themselves.
Her assessment seemed to warn that if there was an epidemic of pain, it was partly driven by the cure. On top of that, there was evidence that the drugs were toxic. Then came the conclusion that stuck a dagger into the heart of the campaign for wider opioid prescribing. “Whereas it was previously thought that unlimited dose escalation was at least safe, evidence now suggests that prolonged, high-dose opioid therapy may be neither safe nor effective,” she wrote.
Ballantyne was also increasingly aware that the claim that pain neutralised the risk of addiction was false. Quantifying addiction, and who may be vulnerable, is notoriously difficult. Ballantyne, like a lot of doctors, estimated that between 10 and 15% of the population is vulnerable, but that it depends on the substance and circumstances. What she was certain of was that Purdue’s high-strength pill, OxyContin, had been a game changer. “The long-acting opiates suddenly put much higher doses into people’s hands and much more of it, and taking it around the clock made them dependent on it.”
From her research, Ballantyne concluded that OxyContin supercharged what was already widespread dependence on weaker opioid pills by drawing a new group of people into the category at risk of addiction and death. The danger was compounded by OxyContin’s failure to live up to its promise of holding pain at bay for 12 hours. For some patients, it wore off after eight, causing them to take three pills a day instead of two, greatly increasing their overall dose of narcotic and with it the risk of addiction.
Ballantyne thought the article would at least cause her profession and the drug industry to take stock of the impact of mass prescribing. By the time the article appeared, the documented death toll from prescription opioids was running at around 8,000 a year.
“When the 2003 New England journal article came out, I thought it was going to make the medical community sit up and say: ‘Wow. These drugs that we’ve been thinking are helping people are not. We have a real problem.’ But the medical community didn’t at all say: ‘Wow,’” Ballantyne said with half a laugh, 15 years later.
“People in my field who had been, like me, taught we have to do this – people who’d been lobbying to try and increase opiate use, like the palliative care physicians – said: ‘What are you doing? We worked so hard to get to this point, and now you’re going to turn it all around. They become so rattled when you suggest you shouldn’t give the opiates – it’s partly people in the pain field and especially people in pharma – because it’s big business.”
Lucas and Ledgerwood had their own study on the impact of opioids in the works. They came to believe the tyranny of the colour-coded smiley faces was costing lives. Years of surgery have given Lucas a healthy respect for pain as a tool for recovery. To suppress it was dangerous. But as large doses of opioids became the norm, the surgeon noted an increasing number of incidents of patients struggling to breathe after routine operations and being moved to intensive care.
Lucas and Ledgerwood visited trauma centres to collect data on deaths before and after the joint commission standards on pain treatment. In 2007, the two doctors published their findings. Before the commission’s dictum, 0.7% of trauma centre patients died from “excess administration of pain medicines”. The death toll rose to 3.6% after the commission’s policies kicked in.
“In each case, administration of sedation led to a change in vital signs or a deterioration in the respiratory status requiring some type of intervention which, in turn, led to a cascade of events resulting in death,” the paper said. Those were only the deaths in which there was little doubt opioids were responsible, and the real toll was almost certainly higher. “Overmedication with sedatives/narcotics … clearly contributed to deaths,” the study concluded.
Emergency departments became beacons for the opioid dependent, who quickly learned to game the system to get drugs on top of their prescriptions. They turned up feigning pain, knowing harassed medical staff under pressure of time and the commission’s standards were likely to prescribe narcotics and move on without too many questions.
“Some of the old-time nurses, they have that jaundiced look in their eye and say ‘So-and-so’s complaining of pain’. You can tell by the look in their eye that they don’t think it’s justified that they get any more medicine,” said Lucas. “The younger nurses, they say we have to treat this pain – because they’ve been indoctrinated – they’ve got to get rid of the pain. God forbid you don’t get rid of the pain. That would be like a mortal sin.”
But there was a price for resisting the pressure to prescribe ever higher doses of pain relief.
Lucas was knocked back in surprise, and then infuriated, to be summoned to appear before his hospital’s ethics committee after a nurse reported him for failing to provide adequate pain treatment.
The surgeon’s longstanding patients included Gail Purton, the wife of a well-known Michigan radio personality. Lucas operated on Purton a few times, and she was back for surgery after her ovarian cancer spread. “It was a big operation. Cut off all sorts of cancer.” The next day, a nurse asked Purton if she was in pain. Purton said she was. The nurse reported Lucas for failing to properly address a patient’s pain. “I got reported because I wasn’t giving her enough pain medicine. She had a big cut from here to here,” Lucas said, running his finger across the front of his shirt and scoffing at the idea that she could be pain-free after an operation like that.
The surgeon responded with a five-page letter to the ethics committee chairman, whom he happened to have trained, challenging the questioning of his professional judgment. Purton wrote her own letter, praising Lucas’s care and saying that she never expected not to have pain after a major operation.
The case was dropped, but it was not an isolated incident. Lucas has worked closely with another surgeon, Anna Ledgerwood, since 1972. She too was hauled before the ethics committee on more than one occasion, on the same charge. It cleared Ledgerwood, but Lucas said more junior surgeons buckled to the pressure to administer opioids just to stay out of trouble.
Lucas regarded the new pain orthodoxy as a growing tyranny. He also thought it was killing patients. He began to collect his own data.
As the joint commission was pushing out its new standards for pain treatment in the early 2000s, the industry was driving a parallel effort to influence the prescribing habits of doctors in small clinics and private practices across the country. Many were still hesitant to prescribe narcotics, in part because of fear of legal liability for overdose or addiction.
The American Pain Society and Haddox, who was by then working for Purdue Pharma, were instrumental in writing a policy document reassuring doctors they would not face disciplinary action for prescribing narcotics, even in large quantities. The industry latched on to the Federation of State Medical Boards because of its influence over health policy individual US states which regulate how doctors practise medicine.
In 2001, Purdue Pharma funded the distribution of new pain treatment guidelines drawn up by the FSMB that sounded many of the same themes as the standards written by the joint commission.
The document picked up on Haddox’s pseudo-addiction theory. “Physicians should recognise that tolerance and physical dependence are normal consequences of sustained use of opioid analgesics and are not synonymous with addiction,” it said.
The FSMB pressed state medical boards to adopt the guidelines and to reassure doctors that adhering to them would diminish the likelihood of disciplinary action.
Over the following decade, the FSMB took close to $2m (£1.52m) from the drug industry, which mostly went to promote the guidelines and to finance a book, Responsible Opioid Prescribing, written with the oversight and advice of a clutch of doctors who were strong advocates of wider use of prescription narcotics. The book was sold to state medical boards and health departments for distribution to physicians, clinics and hospitals. The drug industry paid for the publication but the FSMB kept the $270,000 profits from sales.
Within a few years, the model guidelines were adopted in full or in part by 35 states, and the floodgates were open to mass prescribing of what Drug Enforcement Administration agents came to call “heroin in a pill”. Opioids were soon the default treatment even for relatively minor pain. Dentists gave them to teenagers after pulling their wisdom teeth. Not just one or two days’ worth of pills, but a fortnight or a month’s worth, which, if they did not draw the intended recipient in, frequently sat in the medicine cabinet waiting to be discovered by someone else in the family. The lack of caution in prescribing left an impression among the users that the drugs were harmless, and some people shared them with others as easily as they might an aspirin. Prescribing escalated year on year. So did profits. OxyContin sales passed $1bn a year in 2000. Three years later they were twice that. Other opioid makers were pulling in huge profits too.
By the time the FSMB guidelines were landing in doctors’ inboxes in the early 2000s, Ballantyne had reached her own conclusions about the impact of escalating opioid prescribing. In 2003, she co-authored an article in the New England Journal of Medicine highlighting the dearth of comprehensive trials and saying that two important questions remained unanswered even as mass prescribing of opioids took off. Do they work long term? Are higher doses safe to take year after year? The drug industry and opioid evangelists said yes, but where was the evidence for it?
Ballantyne wrote that there was evidence that putting some patients on serial prescriptions of strong opioids has the opposite of the intended effect. High doses not only build up a tolerance to the drug, but cause increased sensitivity to pain. The drugs were defeating themselves.
Her assessment seemed to warn that if there was an epidemic of pain, it was partly driven by the cure. On top of that, there was evidence that the drugs were toxic. Then came the conclusion that stuck a dagger into the heart of the campaign for wider opioid prescribing. “Whereas it was previously thought that unlimited dose escalation was at least safe, evidence now suggests that prolonged, high-dose opioid therapy may be neither safe nor effective,” she wrote.
Ballantyne was also increasingly aware that the claim that pain neutralised the risk of addiction was false. Quantifying addiction, and who may be vulnerable, is notoriously difficult. Ballantyne, like a lot of doctors, estimated that between 10 and 15% of the population is vulnerable, but that it depends on the substance and circumstances. What she was certain of was that Purdue’s high-strength pill, OxyContin, had been a game changer. “The long-acting opiates suddenly put much higher doses into people’s hands and much more of it, and taking it around the clock made them dependent on it.”
From her research, Ballantyne concluded that OxyContin supercharged what was already widespread dependence on weaker opioid pills by drawing a new group of people into the category at risk of addiction and death. The danger was compounded by OxyContin’s failure to live up to its promise of holding pain at bay for 12 hours. For some patients, it wore off after eight, causing them to take three pills a day instead of two, greatly increasing their overall dose of narcotic and with it the risk of addiction.
Ballantyne thought the article would at least cause her profession and the drug industry to take stock of the impact of mass prescribing. By the time the article appeared, the documented death toll from prescription opioids was running at around 8,000 a year.
“When the 2003 New England journal article came out, I thought it was going to make the medical community sit up and say: ‘Wow. These drugs that we’ve been thinking are helping people are not. We have a real problem.’ But the medical community didn’t at all say: ‘Wow,’” Ballantyne said with half a laugh, 15 years later.
“People in my field who had been, like me, taught we have to do this – people who’d been lobbying to try and increase opiate use, like the palliative care physicians – said: ‘What are you doing? We worked so hard to get to this point, and now you’re going to turn it all around. They become so rattled when you suggest you shouldn’t give the opiates – it’s partly people in the pain field and especially people in pharma – because it’s big business.”
Lucas and Ledgerwood had their own study on the impact of opioids in the works. They came to believe the tyranny of the colour-coded smiley faces was costing lives. Years of surgery have given Lucas a healthy respect for pain as a tool for recovery. To suppress it was dangerous. But as large doses of opioids became the norm, the surgeon noted an increasing number of incidents of patients struggling to breathe after routine operations and being moved to intensive care.
Lucas and Ledgerwood visited trauma centres to collect data on deaths before and after the joint commission standards on pain treatment. In 2007, the two doctors published their findings. Before the commission’s dictum, 0.7% of trauma centre patients died from “excess administration of pain medicines”. The death toll rose to 3.6% after the commission’s policies kicked in.
“In each case, administration of sedation led to a change in vital signs or a deterioration in the respiratory status requiring some type of intervention which, in turn, led to a cascade of events resulting in death,” the paper said. Those were only the deaths in which there was little doubt opioids were responsible, and the real toll was almost certainly higher. “Overmedication with sedatives/narcotics … clearly contributed to deaths,” the study concluded.
A memorial in Washington DC, consisting of 22,000 engraved white pills representing the face of someone lost to a prescription opioid overdose in 2015. Photograph: Mark Wilson/Getty
“I’m convinced that because of the pressures brought to bear by the joint commission, we are killing people,” Lucas told me. The study said the medical staff lived in fear of the joint commission standards which created “great psychological pressure on caregivers” to use narcotics.
In a damning critique, the paper said that the commission’s reliance on pain scales to guide treatment had created an “excessive emphasis on undermedication at the same time ignoring overmedication”. The obsession with ensuring people were not in pain came at the expense of ignoring the dangers of giving large amounts of opioids to people recovering from surgery or serious injury. The drugs may kill the pain but they also risked killing the patient.
The two doctors made no secret of who they blamed for “this preventable cause of death and disability”. “It’s about money. Money has influence, and it influenced the joint commission,” said Lucas.
The surgeon presented the paper to a meeting of the Central Surgical Association and saw it published by the Journal of the American College of Surgeons under the headline “Kindness Kills: The Negative Impact of Pain as the Fifth Vital Sign.”
Afterwards, Lucas got a stream of letters and emails from doctors who recognised the problem. But, unlike Ballantyne, he wasn’t surprised when the policy remained the same. “Did I expect a change? No. It is too ingrained into the medical profession. It’s become financial just like the drug industry is financial. It’s nothing to do with right or wrong. It’s about how the money flows,” he said. “When you write a paper you want there to be unemotional data out there. You want that unemotional data to be analysed and interpreted in one way or the other, but you don’t expect the Renaissance.”
In 2012, nine years after Ballantyne’s cautioning against the mass prescribing of opioids as a quick fix for pain was published in the New England Journal of Medicine, a renowned British pain specialist, Cathy Stannard, called the doctor’s paper “a distant warning bell”, challenging the opening of the floodgates to strong opioids.
Ballantyne continued to collect data and publish ever more detailed insights into the impact of painkillers. A less rapacious drug industry might have paused in its headlong charge to sell opioids, and less blinkered and compliant regulators might have determined that this was the moment to weigh the claims made in favour of permitting such widespread prescribing.
Instead the pharmaceutical companies took the warnings as a challenge to their business interests. Through the 2000s, industry poured money into a political strategy to keep the drugs flowing. It funded front groups and studies to claim that there was indeed an epidemic – but it was of untreated pain. The millions coping with chronic pain were the real victims, the industry said, not the “abusers” hooked on opioids they often bought on the black market or obtained from crooked doctors. That one frequently became the other was conveniently overlooked.
Pharma’s lobbyists worked to persuade Congress and the regulators that to curb opioid prescribing would be to punish the real victims because of the sins of the “abusers”, and it worked. As a result, the devastation ran unchecked for another decade and more. By 2010, doctors in the US were writing more than 200m opioid prescriptions a year. As the prescribing rose, so did the death toll. Last year, more than 72,000 Americans died of drug overdoses, the vast majority from opioids, nearly 10 times the number at the time Ballantyne published her warning.
The head of the FDA at the time OxyContin was approved for distribution two decades ago, Dr David Kessler, later described the opioid crisis as an “epidemic we failed to foresee”. “It has proved to be one of the biggest mistakes in modern medicine,” he said.
Kessler was wrong. It wasn’t a mistake. It was a betrayal.
“I’m convinced that because of the pressures brought to bear by the joint commission, we are killing people,” Lucas told me. The study said the medical staff lived in fear of the joint commission standards which created “great psychological pressure on caregivers” to use narcotics.
In a damning critique, the paper said that the commission’s reliance on pain scales to guide treatment had created an “excessive emphasis on undermedication at the same time ignoring overmedication”. The obsession with ensuring people were not in pain came at the expense of ignoring the dangers of giving large amounts of opioids to people recovering from surgery or serious injury. The drugs may kill the pain but they also risked killing the patient.
The two doctors made no secret of who they blamed for “this preventable cause of death and disability”. “It’s about money. Money has influence, and it influenced the joint commission,” said Lucas.
The surgeon presented the paper to a meeting of the Central Surgical Association and saw it published by the Journal of the American College of Surgeons under the headline “Kindness Kills: The Negative Impact of Pain as the Fifth Vital Sign.”
Afterwards, Lucas got a stream of letters and emails from doctors who recognised the problem. But, unlike Ballantyne, he wasn’t surprised when the policy remained the same. “Did I expect a change? No. It is too ingrained into the medical profession. It’s become financial just like the drug industry is financial. It’s nothing to do with right or wrong. It’s about how the money flows,” he said. “When you write a paper you want there to be unemotional data out there. You want that unemotional data to be analysed and interpreted in one way or the other, but you don’t expect the Renaissance.”
In 2012, nine years after Ballantyne’s cautioning against the mass prescribing of opioids as a quick fix for pain was published in the New England Journal of Medicine, a renowned British pain specialist, Cathy Stannard, called the doctor’s paper “a distant warning bell”, challenging the opening of the floodgates to strong opioids.
Ballantyne continued to collect data and publish ever more detailed insights into the impact of painkillers. A less rapacious drug industry might have paused in its headlong charge to sell opioids, and less blinkered and compliant regulators might have determined that this was the moment to weigh the claims made in favour of permitting such widespread prescribing.
Instead the pharmaceutical companies took the warnings as a challenge to their business interests. Through the 2000s, industry poured money into a political strategy to keep the drugs flowing. It funded front groups and studies to claim that there was indeed an epidemic – but it was of untreated pain. The millions coping with chronic pain were the real victims, the industry said, not the “abusers” hooked on opioids they often bought on the black market or obtained from crooked doctors. That one frequently became the other was conveniently overlooked.
Pharma’s lobbyists worked to persuade Congress and the regulators that to curb opioid prescribing would be to punish the real victims because of the sins of the “abusers”, and it worked. As a result, the devastation ran unchecked for another decade and more. By 2010, doctors in the US were writing more than 200m opioid prescriptions a year. As the prescribing rose, so did the death toll. Last year, more than 72,000 Americans died of drug overdoses, the vast majority from opioids, nearly 10 times the number at the time Ballantyne published her warning.
The head of the FDA at the time OxyContin was approved for distribution two decades ago, Dr David Kessler, later described the opioid crisis as an “epidemic we failed to foresee”. “It has proved to be one of the biggest mistakes in modern medicine,” he said.
Kessler was wrong. It wasn’t a mistake. It was a betrayal.
Monday, 14 August 2017
Don't blame addicts for America's opioid crisis. Here are the real culprits
America’s opioid crisis was caused by rapacious pharma companies, politicians who colluded with them and regulators who approved one opioid pill after another
Chris McGreal in The Guardian
 ‘Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year.’
‘Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year.’

‘This is an almost uniquely American crisis.’
Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year. About half of deaths involved prescription painkillers. Most of those who overdose on heroin or a synthetic opiate, such as fentanyl, first become hooked on legal pills.
This is an almost uniquely American crisis driven in good part by particular American issues from the influence of drug companies over medical policy to a “pill for every ill” culture. Trump’s commission, which called the opioid epidemic “unparalleled”, said the grim reality is that “the amount of opioids prescribed in the US was enough for every American to be medicated around the clock for three weeks”.
The US consumes more than 80% of the global opioid pill production even though it has less than 5% of the world’s population. Over the past 20 years, one federal institution after another lined up behind the drug manufacturers’ false claims of an epidemic of untreated pain in the US. They seem not to have asked why no other country was apparently suffering from such an epidemic or plying opioids to its patients at every opportunity.
With the pharmaceutical lobby’s money keeping Congress on its side, regulations were rewritten to permit physicians to prescribe as many pills as they wanted without censure. Indeed, doctors sometimes found themselves hauled before ethics boards for not supplying enough.
It’s an epidemic because we have a business model for it. Follow the money
Unlike most other countries, the US health system is run as an industry not a service. That gives considerable power to drug manufacturers, medical providers and health insurance companies to influence policy and practices.
Too often, their bottom line is profits not health. Opioid pills are far cheaper and easier than providing other forms of treatment for pain, like physical therapy or psychiatry. As Senator Joe Manchin of West Virginia told the Guardian last year: “It’s an epidemic because we have a business model for it. Follow the money. Look at the amount of pills they shipped in to certain parts of our state. It was a business model.”
But the system also gives a lot of power to patients. People coughing up large amounts of money in insurance premiums and co-pays expect results. They are, after all, more customer than patient. Doctors complain of patients who arrive expecting a pill to resolve medical conditions without taking responsibility for their own health by eating better or exercising more.
In particular, the idea has taken hold, pushed by the pharmaceutical industry, that there is a right to be pain free. Other countries pursue strategies to reduce and manage pain, not raise expectations that it can simply be made to disappear. In all of this, regulators became facilitators. The Food and Drug Administration approved one opioid pill after another.
The Food and Drug Administration approved one opioid pill after another.
As late as 2013, by which time the scale of the epidemic was clear, the FDA permitted a powerful opiate, Zohydro, onto the market over the near unanimous objection of its own review committee. It was clear from the hearing that doctors understood the dangers, but the agency appeared to have put commercial considerations first.
US states long ago woke up to the crisis as morgues filled, social services struggled to cope with children orphaned or taken into care, and the epidemic took an economic toll. Police chiefs and local politicians said it was a social crisis not a law and order problem.
Some state legislatures began to curb mass prescribing. All the while they looked to Washington for leadership. They did not get much from Obama or Congress, although legislation approving $1bn on addiction treatment did pass last year. Instead, it was up to pockets of sanity to push back.
Last year, the then director of the Centers for Disease Control, Tom Frieden, made his mark with guidelines urging doctors not to prescribe opioids as a first step for chronic or routine pain, although even that got political pushback in Congress where the power of the pharmaceutical lobby is not greatly diminished.
There are also signs of a shift in the FDA after it pressured a manufacturer into withdrawing an opioid drug, Opana, that should never have been on sale in the first place. It was initially withdrawn in the 1970s, but the FDA permitted it back on to the market in 2006 after the rules for testing drugs were changed. At the time, many accused the pharmaceutical companies of paying to have them rewritten.
Trump’s opioid commission offered hope that the epidemic would finally get the attention it needs. It made a series of sensible if limited recommendations: more mental health treatment people with a substance abuse disorder and more effective forms of rehab.
Trump finally got around to saying that the epidemic is a national emergency on Thursday after he was criticised for ignoring his own commission’s recommendation to do so. But he reinforced the idea that the victims are to blame with an offhand reference to LSD.
Real leadership is still absent – and that won’t displease the pharmaceutical companies at all.
Chris McGreal in The Guardian
 ‘Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year.’
‘Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year.’
Of all the people Donald Trump could blame for the opioid epidemic, he chose the victims. After his own commission on the opioid crisis issued an interim report this week, Trump said young people should be told drugs are “No good, really bad for you in every way.”
The president’s exhortation to follow Nancy Reagan’s miserably inadequate advice and Just Say No to drugs is far from useful. The then first lady made not a jot of difference to the crack epidemic in the 1980s. But Trump’s characterisation of the source of the opioid crisis was more disturbing. “The best way to prevent drug addiction and overdose is to prevent people from abusing drugs in the first place,” he said.
That is straight out of the opioid manufacturers’ playbook. Facing a raft of lawsuits and a threat to their profits, pharmaceutical companies are pushing the line that the epidemic stems not from the wholesale prescribing of powerful painkillers - essentially heroin in pill form - but their misuse by some of those who then become addicted.
The amount of opioids prescribed in the US was enough for every American to be medicated 24/7 for three weeks”
In court filings, drug companies are smearing the estimated two million people hooked on their products as criminals to blame for their own addiction. Some of those in its grip break the law by buying drugs on the black market or switch to heroin. But too often that addiction began by following the advice of a doctor who, in turn, was following the drug manufacturers instructions.
Trump made no mention of this or reining in the mass prescribing underpinning the epidemic. Instead he played to the abuse narrative when he painted the crisis as a law and order issue, and criticised Barack Obama for scaling back drug prosecutions and lowering sentences.
But as the president’s own commission noted, this is not an epidemic caused by those caught in its grasp. “We have an enormous problem that is often not beginning on street corners; it is starting in doctor’s offices and hospitals in every state in our nation,” it said.
The president’s exhortation to follow Nancy Reagan’s miserably inadequate advice and Just Say No to drugs is far from useful. The then first lady made not a jot of difference to the crack epidemic in the 1980s. But Trump’s characterisation of the source of the opioid crisis was more disturbing. “The best way to prevent drug addiction and overdose is to prevent people from abusing drugs in the first place,” he said.
That is straight out of the opioid manufacturers’ playbook. Facing a raft of lawsuits and a threat to their profits, pharmaceutical companies are pushing the line that the epidemic stems not from the wholesale prescribing of powerful painkillers - essentially heroin in pill form - but their misuse by some of those who then become addicted.
The amount of opioids prescribed in the US was enough for every American to be medicated 24/7 for three weeks”
In court filings, drug companies are smearing the estimated two million people hooked on their products as criminals to blame for their own addiction. Some of those in its grip break the law by buying drugs on the black market or switch to heroin. But too often that addiction began by following the advice of a doctor who, in turn, was following the drug manufacturers instructions.
Trump made no mention of this or reining in the mass prescribing underpinning the epidemic. Instead he played to the abuse narrative when he painted the crisis as a law and order issue, and criticised Barack Obama for scaling back drug prosecutions and lowering sentences.
But as the president’s own commission noted, this is not an epidemic caused by those caught in its grasp. “We have an enormous problem that is often not beginning on street corners; it is starting in doctor’s offices and hospitals in every state in our nation,” it said.

‘This is an almost uniquely American crisis.’
Opioids killed more than 33,000 Americans in 2015 and the toll was almost certainly higher last year. About half of deaths involved prescription painkillers. Most of those who overdose on heroin or a synthetic opiate, such as fentanyl, first become hooked on legal pills.
This is an almost uniquely American crisis driven in good part by particular American issues from the influence of drug companies over medical policy to a “pill for every ill” culture. Trump’s commission, which called the opioid epidemic “unparalleled”, said the grim reality is that “the amount of opioids prescribed in the US was enough for every American to be medicated around the clock for three weeks”.
The US consumes more than 80% of the global opioid pill production even though it has less than 5% of the world’s population. Over the past 20 years, one federal institution after another lined up behind the drug manufacturers’ false claims of an epidemic of untreated pain in the US. They seem not to have asked why no other country was apparently suffering from such an epidemic or plying opioids to its patients at every opportunity.
With the pharmaceutical lobby’s money keeping Congress on its side, regulations were rewritten to permit physicians to prescribe as many pills as they wanted without censure. Indeed, doctors sometimes found themselves hauled before ethics boards for not supplying enough.
It’s an epidemic because we have a business model for it. Follow the money
Unlike most other countries, the US health system is run as an industry not a service. That gives considerable power to drug manufacturers, medical providers and health insurance companies to influence policy and practices.
Too often, their bottom line is profits not health. Opioid pills are far cheaper and easier than providing other forms of treatment for pain, like physical therapy or psychiatry. As Senator Joe Manchin of West Virginia told the Guardian last year: “It’s an epidemic because we have a business model for it. Follow the money. Look at the amount of pills they shipped in to certain parts of our state. It was a business model.”
But the system also gives a lot of power to patients. People coughing up large amounts of money in insurance premiums and co-pays expect results. They are, after all, more customer than patient. Doctors complain of patients who arrive expecting a pill to resolve medical conditions without taking responsibility for their own health by eating better or exercising more.
In particular, the idea has taken hold, pushed by the pharmaceutical industry, that there is a right to be pain free. Other countries pursue strategies to reduce and manage pain, not raise expectations that it can simply be made to disappear. In all of this, regulators became facilitators. The Food and Drug Administration approved one opioid pill after another.
The Food and Drug Administration approved one opioid pill after another.
As late as 2013, by which time the scale of the epidemic was clear, the FDA permitted a powerful opiate, Zohydro, onto the market over the near unanimous objection of its own review committee. It was clear from the hearing that doctors understood the dangers, but the agency appeared to have put commercial considerations first.
US states long ago woke up to the crisis as morgues filled, social services struggled to cope with children orphaned or taken into care, and the epidemic took an economic toll. Police chiefs and local politicians said it was a social crisis not a law and order problem.
Some state legislatures began to curb mass prescribing. All the while they looked to Washington for leadership. They did not get much from Obama or Congress, although legislation approving $1bn on addiction treatment did pass last year. Instead, it was up to pockets of sanity to push back.
Last year, the then director of the Centers for Disease Control, Tom Frieden, made his mark with guidelines urging doctors not to prescribe opioids as a first step for chronic or routine pain, although even that got political pushback in Congress where the power of the pharmaceutical lobby is not greatly diminished.
There are also signs of a shift in the FDA after it pressured a manufacturer into withdrawing an opioid drug, Opana, that should never have been on sale in the first place. It was initially withdrawn in the 1970s, but the FDA permitted it back on to the market in 2006 after the rules for testing drugs were changed. At the time, many accused the pharmaceutical companies of paying to have them rewritten.
Trump’s opioid commission offered hope that the epidemic would finally get the attention it needs. It made a series of sensible if limited recommendations: more mental health treatment people with a substance abuse disorder and more effective forms of rehab.
Trump finally got around to saying that the epidemic is a national emergency on Thursday after he was criticised for ignoring his own commission’s recommendation to do so. But he reinforced the idea that the victims are to blame with an offhand reference to LSD.
Real leadership is still absent – and that won’t displease the pharmaceutical companies at all.
Thursday, 12 December 2013
Reclassifying ketamine is more fiddling while the crack pipe burns
Why can't we have an honest conversation about drugs?

Why can't we talk about our history of intoxication? Photograph: guardian.co.uk
Tis the season to be off your head, legally and in a ladylike manner. At the moment there is a lot of focus on the harm that us people (ie, women) do to ourselves with our: "Yay, it's wine o'clock." Or, as the Sun explains: "So many mums open the wine once the kids are in bed. The cork rarely goes back in the bottle."
One might ask why women's lives are so stressful that self-medication is needed, and why alcohol is such an astonishingly cheap way to get wasted. Legally.
I stress legal because the news that government advisers want ketamine reclassified from a class C to B drug is more fiddling while the crack pipe burns. The drug wasn't banned until 2006, but someone who gets caught with it will now face up to five years in prison instead of two. A heavy price, one feels, for the person who wants to anaesthetise themselves of an evening. Send them to prison where drugs are the currency? It's almost as if government advisers don't live in the real world.
Sure, the long-term effects of ketamine (bladder damage) are not nice and I have never doubted that it is dangerous. When I was 16, two boys I knew broke into a veterinary surgery and injected it. The dose was for horses, not humans. They both died stupid, stupid deaths.
Reclassifying it might mean a few students may now think twice. But those who will be thinking really hard are the manufacturers who will design a legal substance that guarantees the effects of ketamine and can be sold online. For this is how prohibition works hand in hand with capitalism and organised crime. Recently, we have all experienced contact highs – cooking up meth (Breaking Bad), cheering on Nigella (coke), Paul Flowers (a vile cocktail of everything and ill- considered banking). We watch Russell Brand's abstinence monologues that do indeed break the barriers of space and time.
There is no joined-up drugs policy. It is rare that I say a good word about George Osborne but, as I have said in the past, I don't care if he took cocaine. Because I don't. And to be fair to Nick Clegg – maybe I really am out of my mind – he admits that in the war on drugs, drugs won, acknowledging that many senior police officers want decriminalisation. Addiction, Clegg declared recently, is a health issue, not a criminal justice one.
Facts remain a dangerous substance in this debate, as Professor David Nutt knows. In 2009, he said that illegal drugs should be classified according to the harm, both social and individual, they cause. Alcohol would certainly have a high classification. Booze and tobacco, he said, were more harmful than LSD, cannabis and ecstasy. So he had to be got rid of, as few politicians ever seem to be able to expand their minds enough to consider actual evidenced-based policy-making.
Decriminalising certain drugs would inevitably mean misuse. But the unsayable thing is that many of us use drugs, legal and illegal, at certain stages in our lives. And enjoy them.
Instead, however, we hand over the trade to organised crime, which is why Mexico is in the state it is now, upping its poppy production massively. We have spent 10 years trying to bomb or bribe away the only cash crop the Afghans can grow (the opium poppy). What do we want them to sell? Cabbages? This year is a record one for the crop, produced mainly in Helmand, so that has really worked.
You may be the sort of person who does not want to drink or take drugs. You may not wish to expand your mind, or lose it. You may not want to connect the handing-out of mood-altering SSRIs (selective serotonin reuptake inhibitors) with kids smoking skunk and mums' little wine clubs. You may think it's no longer cool to neck any pills other than statins. You may want to move to Uruguay, which has just legalised marijuana, though I can't think of anything worse than being in Montevideo with a load of gap yahs. It's not my drug of choice, as I like things that make you want to talk.
I would like the real drug conversation, not the gurning, coked-up, aren't-we-amazing one. Not the one where Tulisa is a threat to civilisation. Why can't we talk about our history of intoxication, personal and political? Those who make the laws that would make me a criminal are not coherent in their logic. They are cowards, afraid of a media that is neither clean nor sober. Drugs, legal and illegal, are a fact of life. Even life-enhancing. There will be casualties of drugs but there are casualties of not facing reality. Both need to be managed. Honestly, I really cannot snort another line of this hypocrisy.
Sunday, 6 October 2013
Rise and shine: the daily routines of history's most creative minds
Benjamin Franklin spent his mornings naked. Patricia Highsmith ate only bacon and eggs. Marcel Proust breakfasted on opium and croissants. The path to greatness is paved with a thousand tiny rituals (and a fair bit of substance abuse) – but six key rules emerge
One morning this summer, I got up at first light – I'd left the blinds open the night before – then drank a strong cup of coffee, sat near-naked by an open window for an hour, worked all morning, then had a martini with lunch. I took a long afternoon walk, and for the rest of the week experimented with never working for more than three hours at a stretch.
This was all in an effort to adopt the rituals of some great artists and thinkers: the rising-at-dawn bit came from Ernest Hemingway, who was up at around 5.30am, even if he'd been drinking the night before; the strong coffee was borrowed from Beethoven, who personally counted out the 60 beans his morning cup required.Benjamin Franklin swore by "air baths", which was his term for sitting around naked in the morning, whatever the weather. And the midday cocktail was a favourite of VS Pritchett (among many others). I couldn't try every trick I discovered in a new book, Daily Rituals: How Great Minds Make Time, Find Inspiration And Get To Work; oddly, my girlfriend was unwilling to play the role of Freud's wife, who put toothpaste on his toothbrush each day to save him time. Still, I learned a lot. For example: did you know that lunchtime martinis aren't conducive to productivity?
As a writer working from home, of course, I have an unusual degree of control over my schedule – not everyone could run such an experiment. But for anyone who thinks of their work as creative, or who pursues creative projects in their spare time, reading about the habits of the successful, can be addictive. Partly, that's because it's comforting to learn that even Franz Kafkastruggled with the demands of his day job, or that Franklin was chronically disorganised. But it's also because of a covert thought that sounds delusionally arrogant if expressed out loud: just maybe, if I took very hot baths like Flaubert, or amphetamines like Auden, I might inch closer to their genius.
Several weeks later, I'm no longer taking "air baths", while the lunchtime martini didn't last more than a day (I mean, come on). But I'm still rising early and, when time allows, taking long walks. Two big insights have emerged. One is how ill-suited the nine-to-five routine is to most desk-based jobs involving mental focus; it turns out I get far more done when I start earlier, end a little later, and don't even pretend to do brain work for several hours in the middle. The other is the importance of momentum. When I get straight down to something really important early in the morning, before checking email, before interruptions from others, it beneficially alters the feel of the whole day: once interruptions do arise, they're never quite so problematic. Another technique I couldn't manage without comes from the writer and consultant Tony Schwartz: use a timer to work in 90-minute "sprints", interspersed with signficant breaks. (Thanks to this, I'm far better than I used to be at separating work from faffing around, rather than spending half the day flailing around in a mixture of the two.)
The one true lesson of the book, says its author, Mason Currey, is that "there's no one way to get things done". For every Joyce Carol Oates, industriously plugging away from 8am to 1pm and again from 4pm to 7pm, or Anthony Trollope, timing himself typing 250 words per quarter-hour, there's a Sylvia Plath, unable to stick to a schedule. (Or a Friedrich Schiller, who could only write in the presence of the smell of rotting apples.) Still, some patterns do emerge. Here, then, are six lessons from history's most creative minds.
1. Be a morning person
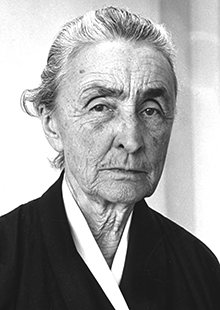 Georgia O'Keeffe: one of a majority of very early morning risers. Photograph: AP
Georgia O'Keeffe: one of a majority of very early morning risers. Photograph: AP
It's not that there aren't successful night owls: Marcel Proust, for one, rose sometime between 3pm and 6pm, immediately smoked opium powders to relieve his asthma, then rang for his coffee and croissant. But very early risers form a clear majority, including everyone from Mozart to Georgia O'Keeffe to Frank Lloyd Wright. (The 18th-century theologian Jonathan Edwards, Currey tells us, went so far as to argue that Jesus had endorsed early rising "by his rising from the grave very early".) For some, waking at 5am or 6am is a necessity, the only way to combine their writing or painting with the demands of a job, raising children, or both. For others, it's a way to avoid interruption: at that hour, as Hemingway wrote, "There is no one to disturb you and it is cool or cold and you come to your work and warm as you write." There's another, surprising argument in favour of rising early, which might persuade sceptics: that early-morning drowsiness might actually be helpful. At one point in his career, the novelist Nicholson Baker took to getting up at 4.30am, and he liked what it did to his brain: "The mind is newly cleansed, but it's also befuddled… I found that I wrote differently then."
Psychologists categorise people by what they call, rather charmingly, "morningness" and "eveningness", but it's not clear that either is objectively superior. There is evidence that morning people are happier and more conscientious, but also that night owls might be more intelligent. If you're determined to join the ranks of the early risers, the crucial trick is to start getting up at the same time daily, but to go to bed only when you're truly tired. You might sacrifice a day or two to exhaustion, but you'll adjust to your new schedule more rapidly.
2. Don't give up the day job
 TS Eliot’s day job at Lloyds bank gave him crucial financial security. Photograph: Hulton Archive/Getty Images
TS Eliot’s day job at Lloyds bank gave him crucial financial security. Photograph: Hulton Archive/Getty Images
"Time is short, my strength is limited, the office is a horror, the apartment is noisy," Franz Kafka complained to his fiancee, "and if a pleasant, straightforward life is not possible, then one must try to wriggle through by subtle manoeuvres." He crammed in his writing between 10.30pm and the small hours of the morning. But in truth, a "pleasant, straightforward life" might not have been preferable, artistically speaking: Kafka, who worked in an insurance office, was one of many artists who have thrived on fitting creative activities around the edges of a busy life. William Faulkner wrote As I Lay Dying in the afternoons, before commencing his night shift at a power plant; TS Eliot's day job at Lloyds bank gave him crucial financial security; William Carlos Williams, a paediatrician, scribbled poetry on the backs of his prescription pads. Limited time focuses the mind, and the self-discipline required to show up for a job seeps back into the processes of art. "I find that having a job is one of the best things in the world that could happen to me," wroteWallace Stevens, an insurance executive and poet. "It introduces discipline and regularity into one's life." Indeed, one obvious explanation for the alcoholism that pervades the lives of full-time authors is that it's impossible to focus on writing for more than a few hours a day, and, well, you've got to make those other hours pass somehow.
3. Take lots of walks
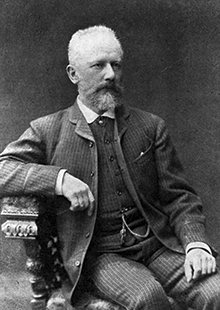 Tchaikovsky 'believed he had to take a walk of exactly two hours a day and that if he returned even a few minutes early, great misfortunes would befall him.' Photograph: Hulton Archive/Getty Images
Tchaikovsky 'believed he had to take a walk of exactly two hours a day and that if he returned even a few minutes early, great misfortunes would befall him.' Photograph: Hulton Archive/Getty Images
There's no shortage of evidence to suggest that walking – especially walking in natural settings, or just lingering amid greenery, even if you don't actually walk much – is associated with increased productivity and proficiency at creative tasks. But Currey was surprised, in researching his book, by the sheer ubiquity of walking, especially in the daily routines of composers, including Beethoven, Mahler, Erik Satie and Tchaikovksy, "who believed he had to take a walk of exactly two hours a day and that if he returned even a few minutes early, great misfortunes would befall him". It's long been observed that doing almost anything other than sitting at a desk can be the best route to novel insights. These days, there's surely an additional factor at play: when you're on a walk, you're physically removed from many of the sources of distraction – televisions, computer screens – that might otherwise interfere with deep thought.
4. Stick to a schedule
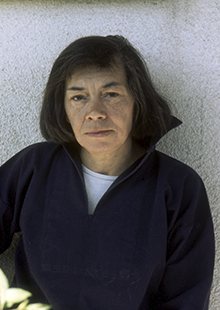 Patricia Highsmith, among others, ate virtually the same thing for every meal, in her case bacon and fried eggs. Photograph: Corbis Sygma
Patricia Highsmith, among others, ate virtually the same thing for every meal, in her case bacon and fried eggs. Photograph: Corbis Sygma
There's not much in common, ritual-wise, between Gustave Flaubert – who woke at 10am daily and then hammered on his ceiling to summon his mother to come and sit on his bed for a chat – and Le Corbusier, up at 6am for his 45 minutes of daily calisthenics. But they each did what they did with iron regularity. "Decide what you want or ought to do with the day," Auden advised, "then always do it at exactly the same moment every day, and passion will give you no trouble." (According to legend, Immanuel Kant's neighbours in Königsberg could set their clocks by his 3.30pm walk.) This kind of existence sounds as if it might require intimidating levels of self-discipline, but on closer inspection it often seems to be a kind of safety net: the alternative to a rigid structure is either no artistic creations, for those with day jobs, or the existential terror of no structure at all.
It was William James, the progenitor of modern psychology, who best articulated the mechanism by which a strict routine might help unleash the imagination. Only by rendering many aspects of daily life automatic and habitual, he argued, could we "free our minds to advance to really interesting fields of action". (James fought a lifelong struggle to inculcate such habits in himself.) Subsequent findings about "cognitive bandwidth" and the limitations of willpower have largely substantiated James's hunch: if you waste resources trying to decide when or where to work, you'll impede your capacity to do the work. Don't consider afresh each morning whether to work on your novel for 45 minutes before the day begins; once you've resolved that that's just what you do, it'll be far more likely to happen. It might have been a similar desire to pare down unnecessary decisions that led Patricia Highsmith, among others, to eat virtually the same thing for every meal, in her case bacon and fried eggs. Although Highsmith also collected live snails and, in later life, promulgated anti-Semitic conspiracy theories, so who knows?
5. Practise strategic substance abuse
 Ayn Rand took Benzedrine. Photograph: New York Times Co/Getty Images
Ayn Rand took Benzedrine. Photograph: New York Times Co/Getty Images
Almost every potential chemical aid to creativity has been tried at some time or another: Auden, Ayn Rand and Graham Greene had their Benzedrine, the mathematician Paul Erdös had his Ritalin (and his Benzedrine); countless others tried vodka, whisky or gin. But there's only one that has been championed near-universally down the centuries: coffee. Beethoven measured out his beans, Kierkegaard poured black coffee over a cup full of sugar, then gulped down the resulting concoction, which had the consistency of mud; Balzac drank 50 cups a day. It's been suggested that the benefits of caffeine, in terms of heightened focus, might be offset by a decrease in proficiency at more imaginative tasks. But if that's true, it's a lesson creative types have been ignoring for ever. Consume in moderation, though: Balzac died of heart failure at 51.
6. Learn to work anywhere
 Agatha Christie didn’t have a desk. Any stable tabletop for her typewriter would do. Photograph: AFP/Getty Images
Agatha Christie didn’t have a desk. Any stable tabletop for her typewriter would do. Photograph: AFP/Getty Images
One of the most dangerous procrastination-enabling beliefs is the idea that you must find exactly the right environment before you can get down to work. "For years, I said if only I could find a comfortable chair, I would rival Mozart," the American composer Morton Feldman recalled. Somerset Maugham had to face a blank wall before the words would come (any other view, he felt, was too distracting). But the stern message that emerges from many other artists' and authors' experiences is: get over yourself. During Jane Austen's most productive years, at Chawton in Hampshire in the 1810s, she wrote mainly in the family sitting-room, often with her mother sewing nearby. Continually interrupted by visitors, she wrote on scraps of paper that could easily be hidden away. Agatha Christie, Currey writes, had "endless trouble with journalists, who inevitably wanted to photograph the author at her desk": a problematic request, because she didn't have one. Any stable tabletop for her typewriter would do.
In any case, absolute freedom from distraction may not be as advantageous as it sounds. One study recently suggested that some noise, such as the background buzz of a coffee shop, may be preferable to silence, in terms of creativity; moreover, physical mess may be as beneficial for some people as an impeccably tidy workspace is for others. The journalistRon Rosenbaum cherishes a personal theory of "competing concentration": working with the television on, he says, gives him a background distraction to focus against, keeping his attentional muscles flexed and strong.
But there is a broader lesson here. The perfect workspace isn't what leads to brilliant work, just as no other "perfect" routine or ritual will turn you into an artistic genius. Flaubert didn't achieve what he did because of hot baths, but through immeasurable talent and extremely hard work. Which is unfortunate, because I'm really good at running baths.
Benzedrine, naps, an early night: an extract from Daily Rituals
Gertrude Stein
In Everybody's Autobiography, Stein confirmed that she had never been able to write for much more than half an hour a day, but added, "If you write a half-hour a day, it makes a lot of writing year by year." Stein and her lifelong partner, Alice B Toklas, had lunch at about noon and ate an early, light supper. Toklas went to bed early, but Stein liked to stay up arguing and gossiping with visiting friends. After her guests finally left, Stein would wake Toklas, and they would talk over the day before both going to sleep.
Ludwig van Beethoven
Beethoven rose at dawn and wasted little time getting down to work. His breakfast was coffee, which he prepared himself with great care: 60 beans per cup. After his midday meal, he embarked on a long walk, which would occupy much of the rest of the afternoon. As the day wound down, he might stop at a tavern to read the newspapers. Evenings were often spent with company or at the theatre, although in winter he preferred to stay at home and read. He retired early, going to bed at 10pm at the latest.
WH Auden
"Routine, in an intelligent man, is a sign of ambition," Auden wrote in 1958. If that's true, the poet was one of the most ambitious men of his generation. He rose shortly after 6am, made coffee and settled down to work quickly, perhaps after taking a first pass at the crossword. He usually resumed after lunch and continued into the late afternoon. Cocktail hour began at 6.30pm sharp, featuring several strong vodka martinis. Then dinner was served, with copious amounts of wine. To maintain his energy and concentration, he relied on amphetamines, taking Benzedrine each morning. At night, he used Seconal or another sedative to get to sleep.
Sylvia Plath
Plath's journal, which she kept from age 11 until her suicide at 30, records a near-constant struggle to find and stick to a productive writing schedule. Only near the end of her life, separated from her husband, Ted Hughes, and taking care of their two small children alone, did she find a routine that worked for her. She was using sedatives to get to sleep, and when they wore off at about 5am, she would get up and write until the children awoke. Working like this for two months in 1962, she produced nearly all the poems of Ariel.
Alice Munro
In the 1950s, as a young mother taking care of two small children, Munro wrote in the slivers of time between housekeeping and child-rearing. When neighbours dropped in, Munro didn't feel comfortable telling them she was trying to work. She tried renting an office, but the garrulous landlord interrupted her and she hardly got any writing done. It ultimately took her almost two decades to put together the material for her first collection, Dance Of The Happy Shades.
David Foster Wallace
"I usually go in shifts of three or four hours with either naps or fairly diverting do-something-with-other-people things in the middle," Wallace said in 1996, shortly after the publication of Infinite Jest. "So I'll get up at 11 or noon, work till two or three." Later, however, he said he followed a regular writing routine only when the work was going badly. "Once it starts to go, it requires no effort. And then actually the discipline's required in terms of being willing to be away from it and to remember, 'Oh, I have a relationship that I have to nurture, or I have to grocery-shop or pay these bills.' "
Ingmar Bergman
"Do you know what moviemaking is?" Bergman asked in a 1964 interview. "Eight hours of hard work each day to get three minutes of film." But it was also writing scripts, which he did on the remote island of Fårö, Sweden. He followed the same schedule for decades: up at 8am, writing from 9am until noon, then an austere meal. "He eats the same lunch," actorBibi Andersson remembered. "It's some kind of whipped sour milk and strawberry jam – a strange kind of baby food he eats with corn flakes." After lunch, Bergman worked from 1pm to 3pm, then slept for an hour. In the late afternoon he went for a walk or took the ferry to a neighbouring island to pick up the newspapers and the mail. In the evening he read, saw friends, screened a movie, or watched TV (he was particularly fond of Dallas). "I never use drugs or alcohol," Bergman said. "The most I drink is a glass of wine and that makes me incredibly happy."
Saturday, 9 June 2012
Kerala plants encyclopedia
Minu Ittiype in Outlook India
One would be forgiven for mistaking Hortus Malabaricus to be a treatise on exotic plants from the Garden of Eden instead of the Garden of Malabar. For author Hendrik Adriaan van Rheede tot Drakenstein’s (then governor of Dutch Malabar, 1670-77) prose on his many journeys into the dense forests of Malabar (in present day Kerala) is almost as lush as the vegetation. Indeed, in one section he describes that he saw such a marvellous variety of flora that it was difficult to find two trees of the same kind in the same forest.
In a flourish of similes, he likens a tree adorned with green creepers to a magnificent palace. (Hardly the stuff one expects in a preface to a plant encyclopedia.) What astonished him no less was how the natives would pick up a few leaves, crush them to use as a balm or eat them to relieve themselves of some ailment.
The secrets of the leaves, roots, berries etc and their effects on the human body were common knowledge in Malabar in the 17th century, passed down orally from one generation to the next. Rheede was intent on documenting this vast trove of traditional knowledge for his fellow Europeans and proceeded to oversee the scientific description and paintings of the medicinal uses of 742 species of flora of Malabar. It was a herculean task which took him 30 years to complete. As governor, he employed 25 experts for the project, including physicians, botanists, painters, engravers, translators and a legion of 200 supporting staff to gather the plants. The Raja of Cochin and the Zamorin of Calicut readily lent their support. The period was not without political intrigue and in between Rheede found himself posted to Batavia in the middle of the project. But he remained ardently faithful to it. The 12 volumes of Hortus were published in Amsterdam between 1678 and 1693.
For over 300 years the Hortus volumes remained in relative obscurity due to a linguistic barrier: it was written in Old Latin and there was none well versed both in Old Latin and the plant kingdom to decipher it. In 1968, K.S. Manilal, a botany scholar and taxonomist, finally undertook the arduous task of studying Latin for 12 years, collected over 400 species of the mentioned plants and decoded Hortus. The project took 35 years of his life, but an English translation was published in 2003 (published by Kerala University) with a Malayalam edition coming out in 2008.
A comprehensive analysis of the Hortus also throws up some uncomfortable questions, some of which have already got the state’s intelligentsia talking. Like the case of the Hortus’s main contributor, a hereditary Ezhava vaidyan (physician) named Itty Achuthan, who was at the time forbidden from using the official written form of Malayalam, vattezhuthu, because he was not from the upper caste. His certificate in kolezhuthu, published in the Hortus, is a testament to this though, ironically, he was the chief protagonist in the documentation. So Hortus, besides documenting the flora, is also a subverted commentary on the culture, linguistics and social structure of the period. The record shows that initially three Saraswat Brahmins—Ranga Bhatt, Vinayak Pandit and Appu Bhatt—gymnosophists well versed in the classic medical texts, were initially employed to assist in identifying the plants. But when Van Rheede found that the Brahmins relied on their servants for physical verification of the plants he found Itty Achuthan far more invaluable. (In a sense, through the encyclopaedia he created, for the first time, an unimaginable inter-caste collaboration.) Achuthan, a descendant of Kollatt vaidyans, had inherited certain ancient palm leaf manuscripts which set out in detail the medicinal use of various plants. During his time, he was considered the most knowledgeable man in the field.
Commemorating the 333rd year of the Hortus, historians now believe it is the only authentic source of the ancient ethno-medical knowledge of Kerala, pre-dating even Ayurveda. As Dr B. Ekbal, former Kerala University V-C, puts it, “It was a decentralised medical practice that was Dravidian and predated ayurveda. Almost like an internal colonisation, later Ayurvedic practitioners appropriated this knowledge.” Today’s Ayurveda doctors are not too sure about this theory, saying their system is codified and argue that the medicinal properties described in Hortus are based mostly on folklore. Dr K. Anilkumar, executive director of Kerala Ayurveda Ltd, says, “We need to study Hortus to ascertain its efficacy. Like it’s mentioned that the bark of the coconut tree can be used to cure liver diseases. We’ll need research to see if there’s any truth to it.”
Kerala’s traditional knowledge of the curative powers of plants has eroded over the years but with the translation of Hortus an intangible heritage has once again become accessible. Some of the plants mentioned have become extinct, others unidentifiable. Even the health of the forests has declined, with trees now reduced to pygmies: the biggest kokum or kodampuli tree of today would at most fill a man’s armspan today but the book has instances of a similar tree’s girth “filling the embrace of two men”. Hortus is a repository of medical treasures as well as insights: who knew the oil of the common brinjal taken with opium has the potent effect of poison?
Subscribe to:
Comments (Atom)